
Chronic Hepatitis C may primarily be associated with the liver, but its effects can ripple out to other vital organs in the body, the respiratory system included. Often, people overlook the intricate ways in which this viral infection can impact their overall well-being. For those living with this chronic illness, understanding how it might affect lung health is vital.
Diving into the relationship between Hepatitis C and respiratory health reveals a fascinating yet concerning link. This not only sheds light on potential complications but also opens the door for better management strategies. Addressing these health issues requires awareness, education, and a proactive approach to care.
- Understanding Chronic Hepatitis C
- Linking Liver and Lung Health
- Respiratory Complications
- Management and Care Tips
- Patient Stories and Experiences
- Future Research and Developments
Understanding Chronic Hepatitis C
Chronic Hepatitis C is a persistent infection caused by the Hepatitis C virus (HCV), a bloodborne pathogen that primarily targets the liver. The virus was first discovered in 1989, and since then, it has been a significant public health issue impacting millions worldwide. The disease is characterized by its stealthy nature; many people harbor the virus for years without showing any symptoms, which complicates early detection and intervention. Once the virus finds a host, it begins by entering liver cells and using their machinery to replicate, often leading to liver inflammation and damage.
Although the liver can regenerate to some extent, ongoing inflammation caused by HCV can eventually result in scarring known as fibrosis. Over time, this scarring can become extensive, leading to cirrhosis, a severe condition where liver function is severely compromised. Notably, individuals with chronic Hepatitis C may not exhibit any obvious symptoms until the disease becomes advanced. When symptoms do manifest, they may include fatigue, jaundice, and abdominal pain, which are unfortunately nonspecific and easily attributed to other conditions.
According to the World Health Organization, approximately 71 million people globally are infected with chronic Hepatitis C. This highlights the public health burden of the disease and underscores the need for improved screening and treatment efforts. Interestingly, the path to infection often begins with activities that involve blood-to-blood contact, such as unsterile medical practices or shared needles among intravenous drug users. Given the potential for liver disease to progress into life-threatening conditions like liver cancer or end-stage liver failure, timely identification and management of hepatitis C are crucial.
Aware of these potential risks, recent decades have seen significant advances in treatment options available for Hepatitis C. Antiviral medications, known as direct-acting antivirals (DAAs), have transformed the landscape of care, offering high cure rates with less severe side effects than older therapies. Despite these advances, many individuals are undiagnosed and untreated, emphasizing the need for continued education and outreach. The development of these therapies has been hailed as one of the great achievements in modern medicine, reflecting the power of sustained research and collaboration.
In the words of Dr. John Ward, Director of the Coalition for Global Hepatitis Elimination, "We have all the tools needed to stop this disease, and what we need now is the commitment to use them."
Efforts to combat the spread of Hepatitis C include not only medical treatment but also public health initiatives aimed at reducing exposure risks. These initiatives often focus on improving the safety of healthcare facilities, ensuring access to clean syringes, and promoting regular screening for at-risk populations. As our understanding of Hepatitis C continues to evolve, so too does our ability to combat this chronic disease and reduce its impact on global health, marking an era of hope and promise against a previously formidable adversary.
Linking Liver and Lung Health
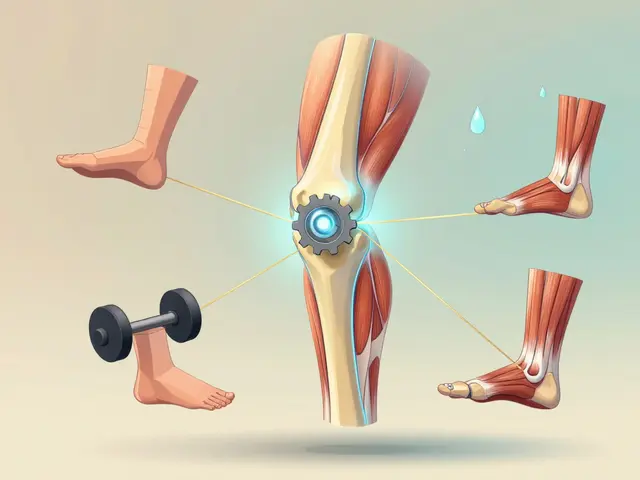
The association between the liver disease caused by Hepatitis C and respiratory health is both complex and often overlooked. The liver, a vital organ responsible for numerous body functions including detoxification and metabolism, can influence various bodily systems when it is compromised. In the context of chronic Hepatitis C, where the liver is under persistent viral assault, there are trickle-down effects on the lungs that can materialize in surprising ways. For instance, when the liver struggles to filter out toxins efficiently due to this infection, these toxins can accumulate in the blood and eventually affect the respiratory system, which is tasked with filtering the air we breathe.
There is also the role of inflammation to consider. Chronic inflammation is a hallmark of long-term Hepatitis C infection, and this inflammatory response doesn’t just restrict itself to the liver. Inflammation can seep into the bloodstream and impact lung tissues, potentially leading to respiratory symptoms such as cough, shortness of breath, or even conditions like pulmonary fibrosis. A study published in the Journal of Infectious Diseases highlighted that patients with chronic Hepatitis C are more likely to experience respiratory issues, underscoring the need for a holistic approach to management. These findings reflect the importance of recognizing and addressing respiratory symptoms early to prevent further complications.
Understanding the pathways through which Hepatitis C affects the lungs isn’t just academic—it has practical implications for healthcare providers who need to develop comprehensive treatment plans. Acknowledging this connection means patients can receive timely interventions that aren’t solely focused on the liver but also consider potential respiratory challenges. As awareness grows, more studies are beginning to investigate how antiviral treatments for Hepatitis C could also yield benefits for lung health. Currently, medical professionals are exploring diverse strategies to mitigate the impact on the respiratory system, which often involves partnering closely with pulmonologists.
“The multiple organ systems involved in chronic Hepatitis C infections make it imperative to adopt multidisciplinary care approaches,” said Dr. Alice Gomez, a specialist in infectious diseases, highlighting the interconnectedness of bodily systems.
For those living with chronic Hepatitis C, becoming informed about the potential respiratory implications is an essential step in advocating for their health. While this virus predominantly targets the liver, its ripple effects underscore the body's interconnected nature. Encouragingly, raising patient awareness and improving collaboration between hepatologists and respiratory specialists can markedly enhance outcomes. As we enhance our understanding of these connections, innovative treatment strategies are on the horizon, which promise not just improved liver health but also preserved and appropriate respiratory function

Respiratory Complications
Chronic Hepatitis C is traditionally associated with the liver, but it strategically orchestrates its chaos across a variety of bodily systems, including the respiratory network. This connection might at first seem tenuous, yet for some patients, the impact on lung health can be remarkably significant. Medical professionals and researchers continue to explore these intertwined relationships, often uncovering a web more intricate than expected. Respiratory problems linked to Hepatitis C tend to manifest as various forms of lung disease or respiratory distress, challenging both patients and caregivers alike. Understanding these complications amid the veiled complexity of viral illnesses has become a subject of concern and focus, drawing attention to the need for comprehensive patient care.
In many cases, individuals with chronic Hepatitis C report experiencing symptoms such as a persistent cough, unexplained shortness of breath, or wheezing, which can be indicative of underlying respiratory issues. Researchers have drawn connections between the virus and conditions like asthma, pulmonary fibrosis, and even lung cancer. Despite significant strides in antiviral treatments, these extrahepatic manifestations persist, ever persistent shadows hinting at deeper internal disruptions. It is hypothesized that the systemic inflammation triggered by the virus aggravates pre-existing conditions or potentially incites new respiratory challenges. Such effects often become subtext in the broader narrative of liver disease, yet deserve their own critical attention.
One fascinating study published in the Journal of Hepatology found that individuals with chronic Hepatitis C face a higher risk of developing chronic obstructive pulmonary disease (COPD) compared to individuals without the infection.
Dr. Isabella Lopez, a leading researcher in the field, highlighted, "The impact of Hepatitis C on pulmonary health is a critical aspect requiring more focus. Our data suggests a clear need for integrated healthcare approaches to simultaneously manage liver and lung health."Such findings emphasize the need for vigilant monitoring of lung function in those diagnosed with the virus. As the understanding of this interplay deepens, healthcare providers are increasingly advocating for a holistic view of treatment, which addresses not just the liver, but the adaptive and sometimes strained dance with coexisting pulmonary conditions.
Mitigating these respiratory complications involves a multifaceted approach, requiring collaboration between hepatologists and pulmonologists. For patients, this might mean regularly scheduled pulmonary function tests, echocardiograms to assess the heart's role, and possibly customized breathing therapies that align with antiviral protocols. Stressing the respiratory system less by controlling environmental triggers like smoke or allergens becomes equally paramount. By acknowledging and proactively addressing these risks, the healthcare community hopes to enhance both longevity and quality of life for those living with chronic Hepatitis C. As research continues, the anticipation is that novel interventions will emerge, potentially altering the landscape of treatment for many who wrestle with this dual challenge.
Management and Care Tips
When grappling with the complexities of Hepatitis C, achieving optimal lung health should be a priority. One essential step involves maintaining a close relationship with healthcare providers who can tailor a comprehensive care plan. Regular check-ups play a crucial role in monitoring not just the liver, but also respiratory functions. Doctors might recommend routine lung function tests to catch any potential issues early. Being proactive in this regard allows for prompt interventions, potentially preventing complications down the line.
Diet is another pillar of management, impacting both liver health and respiratory efficiency. Consuming a balanced diet rich in antioxidants, fruits, and vegetables helps to support the body's immune system. It's advisable to limit the intake of alcohol and fatty foods, as they can exacerbate liver damage, indirectly affecting lung health. Staying hydrated is key, too, as it aids in overall bodily functions, including respiratory processes.
Exercise is often regarded as medicine, and for those with chronic illnesses, it holds transformative power. Engaging in regular physical activity boosts circulation and helps keep the lungs functioning optimally. Incorporating aerobic exercises like walking, swimming, or cycling could enhance respiratory capacity. However, individuals should consult with their healthcare providers to ensure that their exercise routine aligns with their medical condition and capabilities.
"Exercise, nutrition, and adequate hydration form a triad that empowers people to lead better lives despite chronic conditions like Hepatitis C," says Dr. Emily White, a renowned hepatologist.
Stress management also plays a vital role in the holistic care of those affected by Hepatitis C. Chronic stress can weaken the immune system, making the body more vulnerable to infections and illnesses, including those affecting the respiratory system. Techniques such as mindfulness meditation, yoga, and deep breathing exercises can help alleviate stress, providing both mental and physical benefits. Patients might explore different relaxation methods to discover what works for them specifically.
Smoking cessation is non-negotiable for those aiming to protect their respiratory health. Smoking can severely impair lung function and exacerbate any existing respiratory issues. There are numerous resources available, from counseling to nicotine replacement therapies, that can assist individuals in quitting. It's important for patients to realize that quitting smoking can dramatically improve their quality of life, especially when dealing with a complication as significant as liver disease.
Community and support systems cannot be overlooked, either. Many find solace in joining support groups where they can share experiences, challenges, and strategies with others walking a similar path. These networks of empathy and understanding can provide not only emotional support but also practical advice on managing day-to-day challenges. Engaging in such communities can reduce feelings of isolation and empower individuals to take charge of their health.

Patient Stories and Experiences
Living with Hepatitis C is far more than just a medical challenge—it often unfolds as a deeply personal journey filled with resilience, hope, and adaptation. Take the story of Emma, a spirited kindergarten teacher, who found unexpected breathlessness during her daily play sessions with the kids. Initially brushing it off as an innocent side effect of her energetic lifestyle, it wasn't until a persistent cough settled in that alarm bells began to ring. Specialists discovered that the chronic Hepatitis C she had been battling quietly for years had begun affecting her respiratory health, a complication she had never foreseen. Her journey speaks to the importance of understanding how interconnected our bodily systems truly are.
In a different corner of the world, James, a former firefighter, faced a similar battle but with half a dozen additional challenges. His liver disease didn't just limit his physical capabilities, it imposed burdens on his mental well-being as well. Each breath he took during early morning runs seemed to deplete every ounce of energy he had left. For James, it wasn't merely about recognizing the link between liver and lung health, but also finding ways to push through and adapt his lifestyle in a way that didn't compromise his other health priorities. It was here, in this struggle, that he found an unconventional ally in mindfulness practice and light yoga, both of which significantly helped his respiratory health. "Learning to listen and respond to your body is part of the healing journey," James remarked, his words echoing the sentiment of so many in similar situations.
The unique path of each patient offers invaluable lessons, not only in perseverance but also in finding innovative strategies to manage chronic illness. The narrative of Chloe, a young art student, stands out for its emotion and creativity. After experiencing severe fatigue and shortness of breath, she began documenting her experiences through colorful paintings—each stroke a testament to her struggles and triumphs in living with disease. She discovered that by engaging with her creativity, she could navigate the emotional complexities of Hepatitis C, gaining a sense of control over her life and health.
"For some, it’s not just about the medication; it’s about discovering inner peace amidst the chaos," comments Dr. Rachel Stern, a renowned specialist in infectious diseases, acknowledging the diverse coping mechanisms that patients often employ.
These stories highlight a critical reality: no two experiences are the same, even if the condition shared is. While Emma and James discovered their paths through physical activity and mindful practices, Chloe tapped into her artistic side, each cherishing their own path of resilience. Evidence from ongoing research suggests approximately 30% of Hepatitis C patients experience some form of respiratory complication, further amplifying the need for integrated care and empathy. The shared narrative threads from people navigating life with Hepatitis C underscore the importance of community, sharing, and finding personalized methods to enhance quality of life.
Future Research and Developments
As the medical community continues to grapple with the complexities of chronic Hepatitis C and its unexpected implications on respiratory health, ongoing research aims to unravel these mysteries. The connection between liver and lung functionality is highlighted in several studies, urging a growing number of researchers to delve deeply into how viruses traditionally associated with one organ can manifest in others. This expanding field of study is unveiling potential pathways and mechanisms that were once barely acknowledged.
One aspect of ongoing research focuses on the genetic and molecular interactions between the Hepatitis C virus (HCV) and pulmonary tissues. Scientists are exploring how viral proteins might directly influence lung cells, possibly leading to inflammation or fibrosis. Preliminary results are intriguing, showing that certain receptors in pulmonary systems are activated in the presence of HCV, a topic that medical journals are increasingly discussing.
Moreover, clinical trials are actively assessing the effectiveness of current antiviral drugs on respiratory symptoms presented in a subset of patients with chronic Hepatitis C. Researchers are harnessing advancements in biotechnology, aiming to create drugs that are more specifically tailored to tackle both hepatic and respiratory complications simultaneously. The integration of genetic profiling into treatment protocols is promising, offering pathways to customized therapies that could mitigate side effects often observed in broader-spectrum antiviral treatments.
Expanding this research further, the development of comprehensive treatment frameworks that address peripheral conditions caused by Hepatitis C is gaining traction. Physicians are encouraged to adopt a holistic view, one that doesn’t merely isolate the liver as the sole organ of concern. A significant development is the initiative to integrate pulmonologists into multidisciplinary teams for Hepatitis C patients, providing insights into potential respiratory complications and thus improving overall treatment efficacy.
"It's essential for healthcare practitioners to consider the entire bodily ecosystem rather than focusing narrowly on isolated symptoms," explains Dr. Lorna Zhang, a leading researcher in virology and pulmonary medicine. "Only then can we develop therapies that truly enhance patient quality of life."
Future research is poised to explore preventive measures as well, advocating for lung health monitoring as part of regular check-ups in chronic Hepatitis C patients. In parallel, epidemiological studies are underway to assess the long-term impact of existing treatments, gathering data on how these therapies affect lung health over decades. This research is not merely about understanding but also about crafting actionable strategies that can support patients in their everyday lives, combating stigma, and promoting well-rounded health.
Onward-looking, the horizon holds potential not just for better treatment but also for preventive vaccines that can halt Hepatitis C before it begins, safeguarding both liver and lung health. This represents an exceptional period of hope in virology, one where innovation and patient-centric care travel hand in hand. Such developments underscore the necessity of supporting research that unites understanding of chronic conditions like Hepatitis C with broader health outcomes, ensuring the research community continues pushing boundaries for the sake of human health.


17 Comments
Economic health depends on strong liver care and lungs too. We can't ignore the link.
/p>Oh, look, another reminder that the virus that messes up your liver can also make you gasp for air – how utterly convenient, right? Still, it’s good to keep an eye on breathing when you’re dealing with Hep C.
/p>Hey folks, just wanted to point out that the inflammation from chronic Hepatitis‑C isn’t confined to the liver; cytokines can travel through the bloodstream and irritate lung tissue, which explains why some patients develop a nagging cough or shortness of breath. A multidisciplinary approach, pulling in both hepatologists and pulmonologists, can catch these extra‑hepatic symptoms early and improve overall outcomes. It’s also worth noting that antiviral therapy has been shown to reduce systemic inflammation, potentially easing respiratory complaints over time. So if you’re on a DAA regimen, keep talking to your doctor about any new lung‑related symptoms – don’t let them fall through the cracks.
/p>Indeed, the interplay between liver dysfunction and pulmonary health is a classic example of how organ systems communicate, and it’s fascinating to see research highlighting the role of hepatic‑derived toxins, immune‑mediated inflammation, and even altered blood‑gas exchange, all contributing to respiratory symptoms; therefore, routine spirometry and imaging should become standard practice for patients with advanced fibrosis, especially when they present with unexplained dyspnea, persistent cough, or wheezing, which might otherwise be dismissed as unrelated.
/p>Check your lung function if you have Hep C – it can save future trouble.
/p>So you’ve just learned that the virus that quietly hijacks your liver also enjoys meddling with your lungs, because why settle for one organ when you can be a full‑body nuisance? The medical literature, which we all know loves to bury extra‑hepatic findings in the footnotes, actually lists increased rates of chronic bronchitis, COPD, and even pulmonary fibrosis among chronic Hepatitis‑C cohorts. One study even reported a statistically significant rise in the odds of developing interstitial lung disease, which, if you’re not paying attention, could be mistaken for an unrelated allergic reaction. And let’s not forget the cytokine storm that accompanies persistent viral replication; those inflammatory messengers do a fine job of setting fire to lung tissue as well as liver cells. What’s more, the detoxification duties of a compromised liver mean that toxins linger longer in the bloodstream, and the lungs, being the body’s secondary filter, end up doing the heavy lifting. You might notice a chronic cough that refuses to quit, shortness of breath on the slightest exertion, or a wheeze that sounds like a distant train. If you’re on a direct‑acting antiviral regimen, congratulations – you’re probably already on the road to viral clearance, but the damage to your respiratory system may linger, requiring dedicated pulmonary follow‑up. A multidisciplinary team, preferably one that includes a hepatologist, a pulmonologist, and perhaps a physiotherapist, can map out a comprehensive care plan that addresses both liver fibrosis and lung capacity. Lifestyle modifications, such as quitting smoking, avoiding secondhand smoke, and reducing exposure to environmental pollutants, become even more critical when your liver can’t effectively filter out harmful substances. Nutritional support, rich in antioxidants, can also play a supportive role, helping to mitigate oxidative stress that fuels both hepatic and pulmonary inflammation. Regular pulmonary function tests, every six to twelve months, give you a baseline and a trend line to detect any subtle declines before they become debilitating. And don’t underestimate the psychological impact – dealing with a chronic infection and emerging respiratory symptoms can be a mental health burden, so mental health support should be part of the package. The good news is that newer antiviral therapies have dramatically lowered viral loads, which in turn reduces the inflammatory cascade that was once a major driver of extra‑hepatic complications. Future research is already looking at whether adjunct therapies targeting inflammation directly could further protect lung tissue in Hep C patients. Bottom line: treat your liver, but don't forget your lungs; they’re the silent partners in this viral drama, and giving them the attention they deserve could make the difference between a decent quality of life and a constant battle for every breath.
/p>Guess what, the virus that loves to crash your liver also pops over to the lungs for a little vacation – surprise, surprise! 😏 It’s not just a rumor; several trials have shown higher rates of COPD among HCV patients, so keep an eye on that wheeze. And hey, while you’re at it, ask your doc about a spirometry test, because knowing your lung capacity is as essential as knowing your viral load. 🌬️
/p>One must acknowledge the subtle intricacies of hepatic‑pulmonary interplay, yet many disregard the phenomenon as trivial. The literature, albeit replete with data, is often dismissed by the layman as mere anecdote.
/p>Living with a chronic virus feels like carrying an invisible weight; the added breathlessness makes every day a little more oppressive.
/p>It’s a moral failing to ignore the respiratory risks associated with Hepatitis‑C when the data is out there; we have a responsibility to educate, screen, and intervene before a simple cough turns deadly.
/p>Hep C kills more than the liver.
/p>Absolutely, keeping tabs on lung function alongside liver health is a smart move – a simple annual spirometry can catch issues early, and that’s a win for everyone.
/p>Some people think the pharma giants are hiding a secret cure that not only clears the virus but also patches up the lungs, but they keep it buried under layers of "research". The truth is, the same antivirals we have now already reduce systemic inflammation, so the idea of a hidden "dual‑action" pill is more myth than reality. Still, it fuels the imagination and keeps us questioning what’s really being withheld.
/p>Stay hopeful – many patients see both liver and lung improvements after completing their antiviral course, so keep pushing for those follow‑ups and never skip your breathing tests.
/p>Imagine the lungs, once pristine, now whispering alarms with every shallow breath; the liver, once a silent guardian, now a battered battlefield. It’s a cascade of organ‑to‑organ betrayal, a tragic symphony of inflammation, toxins, and relentless viral pressure! Yet, within this darkness, there shines a beacon of multidisciplinary care – hepatologists teaming with pulmonologists, nutritionists, and physiotherapists, stitching together a tapestry of hope. So, dear readers, do not dismiss a cough, do not ignore that lingering wheeze – they are the body’s urgent postcards from the front lines! 🌟
/p>When the virus decides to throw a party in your liver, it invites the lungs as uninvited guests, and the aftermath is nothing short of an epic drama that could rival any Shakespearean tragedy. The key is to intervene early, before the curtain falls on your respiratory function.
/p>Hey all, just a heads‑up – if you’re on HCV meds, ask your doc about a simple breathing test now and then. It’s quick, it’s easy, and it could save you a lot of hassle later. 😊
/p>