
When your kidneys aren’t working right, the medicines you take can turn dangerous-even if they’re safe for everyone else. It’s not just about taking less. It’s about knowing which drugs to avoid, when to change the dose, and what to watch for. For someone with chronic kidney disease (CKD), a simple over-the-counter painkiller or a common antibiotic could land you in the hospital. And yet, most people with kidney problems don’t know this. A 2022 study found that nearly 24% of medications prescribed to CKD patients were given at unsafe doses. That’s not a mistake. It’s a systemic failure.
Why Kidneys Matter for Medicines
Your kidneys don’t just make urine. They filter your blood, removing waste and extra fluid. But they also clear out most drugs. When kidney function drops, those drugs build up. Too much metformin? Risk of lactic acidosis. Too much vancomycin? Hearing loss or kidney damage. Too much ibuprofen? Sudden kidney injury. The problem isn’t the drug itself-it’s the dose.
Doctors used to think lowering blood pressure with ACE inhibitors or ARBs was risky in advanced kidney disease because it raised creatinine. But that’s outdated. The 2024 KDIGO guidelines say: maximize those drugs. A rise in creatinine doesn’t mean harm-it often means the drug is working. Stopping them out of fear actually increases the risk of heart attack, stroke, and kidney failure.
Which Drugs Are Most Dangerous?
Not all medications are created equal when your kidneys are weak. Some are fine. Others? Avoid them like poison.
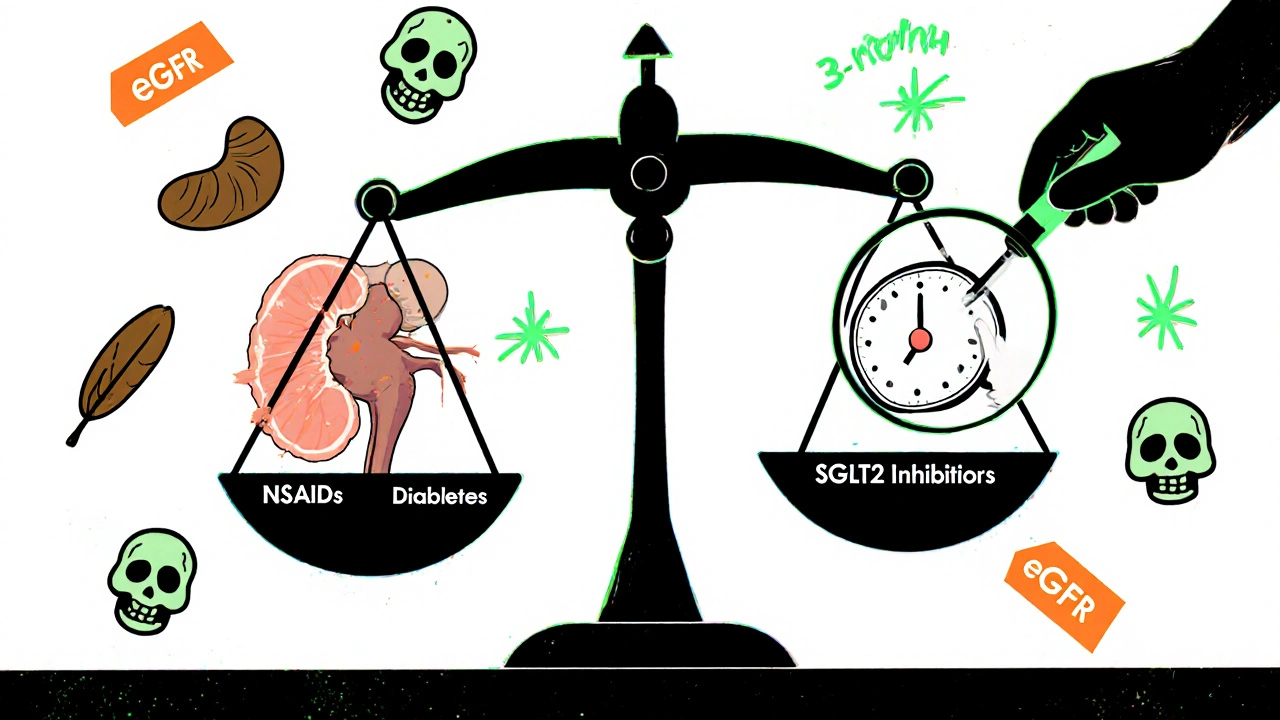
- NSAIDs (ibuprofen, naproxen, celecoxib): These are the #1 cause of preventable kidney injury in CKD patients. Even a few days of use can spike creatinine by 50% or more. One patient on Reddit shared how two Advil sent his creatinine from 3.2 to 5.7 in 48 hours. He ended up in the ER with acute kidney injury.
- Metformin: This diabetes drug is safe for most, but not if your eGFR drops below 30. Between 30 and 45, use it cautiously. Above 45? Usually fine. But many doctors still prescribe it without checking kidney numbers. That’s dangerous.
- Aminoglycosides (gentamicin, tobramycin): Antibiotics that stick around when kidneys fail. They can cause permanent hearing loss or kidney damage. Dosing must be extended-once daily instead of every 8 hours-and trough levels must be checked.
- Sodium phosphate bowel prep: Used before colonoscopies. It can cause acute kidney failure in CKD patients. The 2025 DoD/VA guidelines now recommend polyethylene glycol (PEG) instead-no risk, same results.
- Contrast dye: Used in CT scans. Can trigger contrast-induced nephropathy. If you have CKD, ask if the scan is truly necessary. Hydrate well. Some hospitals now use low-osmolar agents or delay the scan if eGFR is below 45.
Here’s the twist: not all diabetes drugs are risky. SGLT2 inhibitors like dapagliflozin and empagliflozin are actually kidney protectors. They work regardless of kidney function. You don’t adjust the dose-even if your eGFR is 15. In fact, the 2024 KDIGO guidelines now recommend them for all CKD patients with albuminuria, even if they don’t have diabetes. They cut the risk of kidney failure by nearly 40%.
What Is eGFR? And Why It’s Your Most Important Number
eGFR stands for estimated glomerular filtration rate. It’s a number doctors calculate from your creatinine, age, sex, and race. It tells you how well your kidneys are filtering. It’s not perfect-but it’s the best tool we have.
- eGFR ≥90: Normal kidney function
- eGFR 60-89: Mild reduction
- eGFR 30-59: Moderate reduction (Stage 3 CKD)
- eGFR 15-29: Severe reduction (Stage 4)
- eGFR <15: Kidney failure (Stage 5)
Most medications need dose changes when eGFR drops below 60. Some, like metformin, require stopping below 30. Others, like SGLT2 inhibitors, need no change at all. The problem? Many EHR systems don’t alert doctors when a patient’s eGFR changes. A 2022 study in JAMA Internal Medicine found that 23.7% of CKD patients got inappropriate doses because the system didn’t flag it.

How to Stay Safe: A Simple Checklist
You don’t need to be a doctor to protect yourself. Here’s what to do:
- Know your eGFR. Ask for it at every visit. Don’t let them just say “your kidneys are fine.” Ask for the number.
- Keep a current medication list. Include every pill, supplement, and OTC drug. Bring it to every appointment.
- Use one pharmacy. Studies show patients who use a single pharmacy have 42% fewer medication-related kidney injuries. Pharmacists can spot dangerous interactions.
- Ask: “Is this safe for my kidneys?” Before starting any new drug-even a cold medicine or sleep aid.
- Check for kidney-safe alternatives. If you need pain relief, use acetaminophen (Tylenol) instead of NSAIDs. For diabetes, ask about SGLT2 inhibitors or GLP-1 agonists instead of sulfonylureas, which raise hypoglycemia risk.
- Get a quarterly medication review. KDIGO recommends this for all Stage 3-5 CKD patients. If your doctor doesn’t offer it, ask.
What’s New in 2025? The Big Shifts
Medication safety in kidney disease isn’t static. The rules changed recently-and they’re changing again.
- SGLT2 inhibitors are now first-line. Not just for diabetics. For anyone with CKD and protein in their urine (albuminuria). They protect the heart and kidneys, no dose adjustment needed.
- Finerenone is now recommended. This new drug (a non-steroidal mineralocorticoid receptor antagonist) is added when ACE/ARBs aren’t enough-and potassium is under 4.8. It reduces kidney failure risk by another 20%.
- Vancomycin dosing changed. In CKD, the target trough level is now 10-15 mcg/mL, not 15-20. Higher levels increase toxicity without better outcomes.
- Electronic alerts are improving. The Veterans Health Administration reduced inappropriate dosing by 37% after adding eGFR-based alerts to their system. More hospitals are following suit.
What’s Still Missing?
Even with the best guidelines, gaps remain. No one has a perfect dosing chart for end-stage kidney disease (eGFR <15) if you’re not on dialysis. That’s when you need therapeutic drug monitoring-measuring blood levels of drugs like vancomycin or digoxin. But most clinics don’t do it routinely.
Also, most apps and online calculators still use the outdated Cockcroft-Gault formula. The 2024 KDIGO guidelines recommend using CKD-EPI instead. It’s more accurate, especially for women and older adults. Ask your pharmacist which one they use.
And let’s talk about over-the-counter drugs. A 2023 NIDDK survey found that 68% of CKD patients didn’t know which OTC meds were risky. They thought “natural” meant safe. It doesn’t. Herbal supplements like licorice root, creatine, and high-dose vitamin C can harm kidneys. Even some weight-loss teas contain senna or aloe, which cause electrolyte imbalances.
Real Stories, Real Lessons
One patient, ‘CKDSurvivor’ on DaVita, shared how her nephrologist caught her metformin dose was still at 1000 mg twice daily-even though her eGFR had dropped to 38. They switched her to a safer drug before she developed lactic acidosis. She says, “I didn’t know my kidneys had changed. My doctor did. That saved me.”
Another, ‘DialysisDave,’ took ibuprofen for a headache and ended up in the hospital with a creatinine spike from 3.2 to 5.7. He spent 10 days on IV fluids. His kidney function never fully returned. “I thought it was just a painkiller,” he said. “I didn’t know it could kill my kidneys.”
These aren’t rare. They’re preventable.
What You Can Do Today
You don’t have to wait for a guideline update. Start now.
- Call your pharmacy. Ask them to review your entire medication list for kidney safety.
- Write down your latest eGFR and bring it to your next appointment.
- Throw out any NSAIDs you have at home. Replace them with acetaminophen.
- If you have diabetes, ask your doctor: “Am I on an SGLT2 inhibitor? If not, should I be?”
- Set a reminder: every 3 months, ask for a medication review.
Medication safety in kidney disease isn’t about fear. It’s about awareness. It’s about asking the right questions. And it’s about knowing that the same pill that helps your neighbor could hurt you-because your kidneys work differently.
Can I still take ibuprofen if I have kidney disease?
No. NSAIDs like ibuprofen, naproxen, and celecoxib can cause sudden kidney injury in people with CKD-even if you’ve taken them safely before. They reduce blood flow to the kidneys, which can trigger acute kidney failure. Use acetaminophen (Tylenol) instead for pain or fever, and never exceed 3,000 mg per day.
Do all diabetes medications need dose changes in kidney disease?
No. Metformin must be stopped if eGFR falls below 30 and used cautiously between 30-45. Sulfonylureas like glipizide increase hypoglycemia risk and should be avoided. But SGLT2 inhibitors (dapagliflozin, empagliflozin) and GLP-1 agonists (semaglutide, liraglutide) require no dose adjustment, even in advanced kidney disease. In fact, SGLT2 inhibitors are now recommended as first-line therapy for CKD patients with protein in their urine.
What’s the best way to monitor my kidney function at home?
You can’t reliably monitor kidney function at home. eGFR requires a blood test. But you can track symptoms: swelling in ankles, fatigue, nausea, or reduced urine output may signal worsening kidney function. Keep a log and share it with your doctor. The best tool is regular lab work-every 3-6 months if you have CKD stage 3 or higher.
Are herbal supplements safe for people with kidney disease?
Many are not. Supplements like licorice root, creatine, high-dose vitamin C, and certain weight-loss teas contain ingredients that can damage kidneys or cause dangerous electrolyte shifts. Some herbal products are contaminated with heavy metals or hidden pharmaceuticals. Always tell your doctor about every supplement you take-even if you think it’s “natural.”
Why does my doctor want me on an ACE inhibitor even though my creatinine went up?
A rise in creatinine doesn’t mean your kidneys are getting worse-it often means the ACE inhibitor is working. These drugs reduce pressure in the kidney’s filtering units, which protects them long-term. Clinical trials proved that maximum tolerated doses reduce kidney failure and heart attacks-even in advanced CKD. Stopping them because of a creatinine rise is outdated and dangerous.
How often should I get my medications reviewed if I have kidney disease?
At least every 3 months if you have stage 3, 4, or 5 CKD. More often if you’re hospitalized, sick, or your eGFR changes quickly. A medication review means your doctor or pharmacist checks every pill, supplement, and OTC drug to make sure it’s still safe and needed. This simple step prevents 40% of medication-related kidney injuries.
What’s Next?
The future of kidney-safe medication use is moving fast. By 2026, the FDA plans to use real-world data from electronic health records to update dosing guidelines. Pharmacogenomics-testing how your genes affect drug metabolism-is being studied in 17 clinical trials for CKD patients. The goal? Personalized dosing based on your biology, not just your eGFR.
But you don’t need to wait for the future. Right now, you can take control: know your numbers, ask questions, use one pharmacy, and avoid NSAIDs. These steps don’t require a new app or a fancy test. They just require you to speak up.
Your kidneys can’t tell you when something’s wrong. But you can. And that makes all the difference.






14 Comments
Oh honey, let me just say - if your nephrologist is still prescribing NSAIDs to a CKD patient without a signed waiver and a blood oath, they’re practicing medieval medicine with a PowerPoint. I’ve seen patients on ibuprofen for ‘back pain’ while their eGFR hovers at 28. It’s not negligence. It’s arrogance dressed in white coats. And don’t get me started on how hospitals still use contrast dye like it’s 1999. The science is 2024. The practice? Still stuck in the dial-up era. Someone needs to sue the AMA for emotional damages.
/p>i think the gov is hiding somthing about kidney meds… i read on a forum that the pharma compnies pay doc to keep metformin on the list even when its dangerous… also the eGFR thing? its all rigged. they change the race factor to make it look better for black ppl so they dont get transplants. its all connected. i know a guy who got his kidney taken out and the doc said ‘its fine’ then he died. i think its the 5g.
/p>Thank you for posting this!! 🙏 I’ve been trying to explain to my uncle why he can’t just pop Advil like candy since his diagnosis, and this is the clearest thing I’ve found. I printed it out and gave it to his doctor. He actually listened! 😊 If you’re reading this and have CKD - you’re not alone. Small changes save lives. You got this 💪
/p>Of course Americans are still using NSAIDs. You people treat medicine like a grocery store. You want pain gone? Take two. You want your kidneys to stop working? Keep going. In Ireland, we don’t have this problem because we trust our GPs - not some internet guru with a 2024 guideline PDF. You don’t need a PhD to know ibuprofen isn’t for kidneys. It’s common sense. Not rocket science. Stop blaming the system. Blame yourselves.
/p>Just want to say SGLT2 inhibitors are a game changer. My mom’s eGFR was 22 and she’s on dapagliflozin - no dose changes, no side effects, and her albuminuria dropped by 60% in 6 months. The docs were shocked. Also hydration before contrast scans? Non-negotiable. I make my husband drink a liter of water before every CT. He hates it but he’s alive. 💯
/p>Just had a conversation with my nephrologist about this yesterday 😊 She said the same thing about ACE inhibitors - creatinine going up doesn’t mean failure, it means the drug is doing its job. Also, PEG bowel prep? YES. My cousin had contrast-induced AKI last year. Never again. I now ask every specialist: ‘Is this necessary? Can we use a safer alternative?’ It’s not being difficult. It’s being smart. 🙌
/p>you americans are so lazy. in india we dont have this problem because we dont take 10 pills a day. if your kidney is weak you eat dal and roti and drink water. no ibuprofen. no metformin. no contrast. no doctor. just god and nature. you think science can fix everything? look at your obesity crisis. your meds are killing you not your kidneys.
/p>Thank you for writing this. I’ve been managing CKD for 8 years and this is the most accurate, non-alarmist summary I’ve ever read. The part about ACE inhibitors? I wish I’d known that 5 years ago. I stopped mine out of fear and ended up in the ER with heart failure. The guidelines are right - don’t panic, just adapt. And if your doctor doesn’t know this? Find a new one. You deserve better.
/p>From an Indian nephrologist: The real issue is diagnostic arbitrariness. eGFR equations are race-adjusted, which introduces systemic bias. We need population-specific equations. Also, aminoglycosides are still overused in rural hospitals because they’re cheap. We need mandatory renal dosing alerts in EHRs. Until then, patient advocacy is the only safety net. This post nails it.
/p>For anyone reading this and feeling overwhelmed - you’re not failing. You’re learning. This stuff is complicated. I’ve coached dozens of CKD patients through this. Start with one thing: ask your pharmacist to review your med list. They’re the unsung heroes. And if they say ‘it’s fine’ - ask again. You have a right to understand what’s in your body. You’re not a burden. You’re a warrior.
/p>they're lying about the drugs. the FDA knows ibuprofen causes kidney failure but they let it stay on shelves because they get money from the drug companies. also the eGFR is fake. they made it up so they can sell more tests. my neighbor's cousin's dog got sick after a vet gave it ibuprofen and now the vet is in jail. i saw it on youtube.
/p>As a renal pharmacist in Mumbai: The real gap is in tier-2/3 cities where pharmacists dispense NSAIDs without eGFR. We need a mandatory CKD flag in the national pharmacy database. Also, SGLT2 inhibitors are underutilized due to cost - but they’re cost-effective long-term. We’re piloting a subsidized program. If you’re in India and have CKD + albuminuria - ask for dapagliflozin. It’s life-changing.
/p>There’s a quiet revolution happening in nephrology - and most people don’t even know it. We’ve moved from ‘protect the kidney at all costs’ to ‘optimize outcomes holistically.’ That means accepting a slight creatinine rise as a sign of protection, not failure. It means choosing a drug not by its label, but by its effect on mortality, not just labs. It means trusting data over dogma. This isn’t just medicine. It’s a philosophical shift. And it’s beautiful.
/p>My grandma’s on dialysis now. She took ibuprofen for her arthritis for years. Didn’t know it was dangerous. I wish I’d known this sooner. But hey - better late than never. I’m her med manager now. We’ve cut out the NSAIDs, switched to Tylenol (carefully), and she’s on empagliflozin. Her BP’s better, her swelling’s down. I’m not a doctor. I’m just her grandson. But I read. And I listened. You can too. Start small. One pill at a time.
/p>