
When your heart suddenly races to 150 beats per minute or more, it can feel like a roller‑coaster you didn't sign up for. Supraventricular Tachycardia is a rapid heart rhythm that starts above the heart's ventricles, often kicking in without warning. Understanding why it happens and how to keep it at bay can turn a scary episode into something you manage with confidence.
- SVT is an arrhythmia that originates above the ventricles.
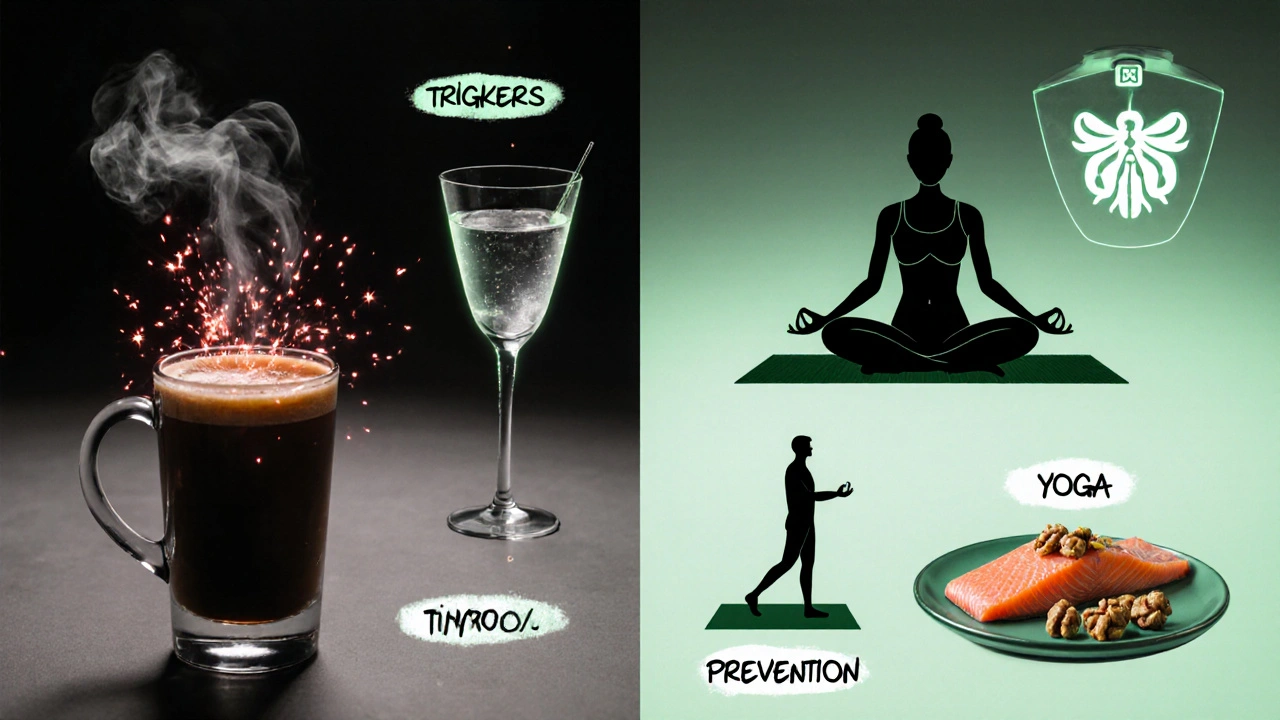
- Age, genetics, caffeine, and certain heart conditions raise the odds.
- Lifestyle tweaks and regular check‑ups can cut the chance of episodes.
- Fast‑acting maneuvers and medicines help stop a sudden flare‑up.
- Seek medical help if symptoms last longer than a few minutes or cause chest pain.
What is Supraventricular Tachycardia?
Arrhythmia refers to any irregular heartbeat, whether too fast, too slow, or erratic is a broad term that includes Supraventricular Tachycardia. In SVT, the electrical impulse that normally travels from the atria (the heart’s upper chambers) to the ventricles (the lower chambers) takes a shortcut or loops back, causing the atria to fire off signals at a breakneck speed. The result is a heartbeat that can jump from 100 up to 250 beats per minute, often feeling like a pounding chest, shortness of breath, or light‑headedness.
Who’s most at risk? Common risk factors
Risk Factor any characteristic, condition, or behavior that increases the likelihood of developing a disease can be split into two buckets: those you can’t change and those you can.
- Age > 40 years - the electrical system naturally slows down.
- Family history - having a close relative with SVT or other arrhythmias doubles the chance.
- Underlying heart disease - previous heart attacks, valve problems, or congenital defects create scar tissue that acts like a shortcut for electrical signals.
- Thyroid overactivity - excess thyroid hormone speeds up the heart’s baseline rhythm.
- Stimulant use - caffeine, nicotine, and certain illegal drugs (e.g., cocaine) temporarily boost heart rate.
- Alcohol bingeing - especially in people with “holiday heart” episodes.
| Category | Risk Factor | Typical Impact |
|---|---|---|
| Non‑modifiable | Age > 40 | Increases baseline susceptibility |
| Non‑modifiable | Family history | Genetic predisposition |
| Non‑modifiable | Congenital heart defects | Structural pathways for re‑entry circuits |
| Modifiable | High caffeine intake | Triggers premature atrial beats |
| Modifiable | Smoking | Elevates catecholamine levels |
| Modifiable | Excess alcohol | Causes transient atrial irritability |
| Modifiable | Uncontrolled hyperthyroidism | Speeds overall heart rate |
How lifestyle choices influence your risk
Lifestyle Modification deliberate changes to daily habits that improve health outcomes can shave years off the chance of an SVT episode.
- Keep caffeine under 200mg per day - roughly one strong coffee. If you notice palpitations after a cup, cut back.
- Quit smoking or switch to nicotine‑free alternatives. Even occasional cigars raise heart‑rate spikes.
- Limit alcohol to no more than two drinks on a single occasion, and avoid bingeing on weekends.
- Stay hydrated. Dehydration lowers blood volume, prompting the heart to work harder.
- Practice stress‑relief techniques - deep breathing, meditation, or yoga - at least 10minutes a day. Stress hormones can act like hidden stimulants.
- Maintain a healthy weight. Excess fat forces the heart to pump more blood, which can trigger arrhythmias.
Medical strategies to prevent episodes
Beta Blocker a class of medication that slows the heart by blocking adrenaline’s effects is often the first prescription for frequent SVT. Common options like atenolol or metoprolol keep the baseline heart rate lower, making it harder for an extra beat to launch a full‑blown episode.
When an episode strikes, a Vagal Maneuver a simple technique that stimulates the vagus nerve to slow the heart can be surprisingly effective. The classic “Valsalva” - a forced exhalation against a closed airway for 15 seconds - stops the rapid rhythm in about 30% of cases.
If medicines and maneuvers don’t cut it, an Electrophysiology Study a diagnostic procedure that maps the heart’s electrical pathways can pinpoint the exact circuit causing SVT. Most patients then undergo catheter ablation, where a tiny probe delivers heat or cold energy to destroy the abnormal pathway, offering a cure in over 95% of cases.
All of these options are best discussed with a Cardiologist a doctor specialized in heart health and rhythm disorders who can tailor treatment to your personal risk profile.
Everyday habits that keep your rhythm steady
- Check your pulse each morning - 60‑100bpm is normal at rest.
- Log any palpitations in a notebook or phone app. Patterns often reveal triggers.
- Get at least 7hours of sleep; sleep deprivation spikes heart‑rate variability.
- Include omega‑3‑rich foods (salmon, walnuts) that support heart cell membranes.
- Schedule an annual cardiac check‑up, especially if you have a family history.

When to call a professional
If a rapid heartbeat lasts more than 5minutes, is accompanied by chest pain, fainting, or shortness of breath that doesn’t improve with rest, treat it as an emergency. Even brief episodes that happen repeatedly should prompt a visit, because early intervention can prevent more dangerous arrhythmias down the line.
Frequently Asked Questions
What exactly triggers a sudden SVT episode?
Common triggers include a surge of caffeine, stress, lack of sleep, alcohol bingeing, and certain medications such as decongestants. In people with scar tissue from prior heart surgery, even a minor premature beat can start a rapid circuit.
Can SVT be cured without medication?
Yes, many patients achieve a permanent cure through catheter ablation, which destroys the abnormal electrical pathway. The procedure has a success rate above 95% and a low complication risk.
Are beta blockers safe for everybody?
Beta blockers are generally safe but can cause fatigue, cold hands, or low blood pressure, especially in people with asthma or severe diabetes. A cardiologist will adjust dosage or suggest alternatives like calcium‑channel blockers if needed.
How often should I monitor my heart rate?
If you’ve never had an episode, a weekly check is fine. Once you’ve experienced SVT, daily monitoring for at least a month helps identify patterns and evaluate treatment effectiveness.
Is exercise risky for someone with SVT?
Moderate aerobic activity (like brisk walking or cycling) is actually protective because it improves overall heart conditioning. Avoid extreme endurance events or high‑intensity interval training until your doctor confirms it’s safe.
If you’ve been diagnosed with Supraventricular Tachycardia, remember that a blend of lifestyle tweaks, timely medical care, and simple at‑home tricks can keep the rhythm steady and your quality of life high.






20 Comments
Just cut your coffee to a single cup a day and you’ll notice the palpitations drop.
/p>Vagal maneuvers are your first line of defense – the Valsalva, the carotid sinus massage, even a good old ice‑cold water splash can break the circuit.
/p>You don’t need fancy equipment; just a few seconds of controlled breath can do the trick.
Keep a quick guide on your phone for when the heart decides to sprint, and practice it in a calm setting so you’re ready.
Consistency in applying these tricks often reduces the need for medication escalation.
People really should think about how their choices affect the heart, its not just a matter of feeling “fine”.
/p>If you keep guzzling caffeine and binge drinking, you’re practically inviting SVT to the party.
Take responsibility and watch the rhythm settle.
Oh sure, because who doesn’t love an unexpected 200‑bpm sprint right after the morning coffee?
/p>Your heart is basically trying to win a speed contest it never signed up for.
The good news? You can actually hit the brakes with a simple breath hold – no need for a superhero cape.
The bad news? Most of us ignore the warning signs until we’re left gasping on the couch.
So maybe next time, give that Valsalva a go before you blame the universe.
Staying hydrated helps keep blood volume stable, which in turn eases the workload on your heart.
/p>Dehydration can trigger extra beats that snowball into SVT.
Aim for at least eight glasses a day, especially if you’re active.
Honestly, the notion that “just live your life” works when your heart decides to rev up is laughable.
/p>You need a plan, not wishful thinking.
Proper meds and a solid vagal routine are non‑negotiable.
I’ve seen many patients struggle with the anxiety that comes after an SVT episode, and the uncertainty can be worse than the rhythm itself.
/p>Keeping a log of triggers – caffeine amount, stress levels, sleep quality – gives concrete data to discuss with your cardiologist.
Over time, you’ll notice patterns and can proactively adjust lifestyle factors.
Exactly, tracking those details turns vague fears into actionable insights.
/p>It also empowers you during appointments, showing the doctor you’re actively managing the condition.
Keep up the diligent note‑taking and you’ll likely see fewer surprise attacks.
Think of your heart as a high‑performance engine; you wouldn’t feed a race car with cheap fuel and expect smooth rides.
/p>Each cup of joe, each night‑out drink, adds a little grit to the combustion chamber.
Trim the excess, and you’ll hear a more harmonious purr rather than a frantic revving.
It’s not about giving up fun, just about fine‑tuning the inputs.
Oh dear, the saga of caffeine‑fueled heart drama continues! 🌪️ You’re right, the heart isn’t a careless teenager; it reacts dramatically to every stimulant you toss its way.
/p>Cutting down isn’t a punishment, it’s the plot twist where the hero finally learns restraint.
Imagine the applause when your pulse settles into a calm rhythm – it’ll be legendary! 😉
Supraventricular tachycardia can feel like your heart switched to turbo mode without warning.
/p>The first step is to recognize the early signs – fluttering, mild chest pressure, or a sudden rush of blood to the head.
Once you notice these, pause and try a slow, deep breath to engage the vagus nerve.
If the heartbeat doesn’t settle, the Valsalva maneuver – a forced exhale against a closed airway for about fifteen seconds – often breaks the cycle.
Many patients report that practicing this technique beforehand makes it more effective during an actual episode.
Beyond acute measures, long‑term management hinges on lifestyle modifications.
Limiting caffeine to less than 200 mg per day, roughly one strong cup of coffee, reduces premature atrial beats that can trigger SVT.
Alcohol intake should be kept moderate; binge drinking is a well‑known catalyst for the so‑called ‘holiday heart’ phenomenon.
Regular exercise, especially moderate aerobic activities like brisk walking or cycling, strengthens the heart’s electrical stability.
Weight management also plays a role, as excess body mass forces the heart to pump more vigorously, increasing arrhythmia risk.
If lifestyle tweaks aren’t enough, beta‑blockers such as metoprolol can lower the baseline heart rate, making it harder for an ectopic beat to spiral into tachycardia.
For those with frequent episodes, an electrophysiology study pinpoints the exact re‑entry circuit.
Catheter ablation, performed by an experienced electrophysiologist, destroys that problematic pathway and offers a cure in the overwhelming majority of cases.
It’s crucial to have regular follow‑up appointments to monitor heart rhythm and adjust therapy as needed.
Finally, keeping a simple diary of symptoms, triggers, and interventions empowers you to spot patterns and discuss them intelligently with your cardiologist.
Interesting how you can turn a medical guide into a philosophical treatise about heartbeats and destiny.
/p>Yet, at the end of the day, if the rhythm doesn’t settle, philosophy won’t save you from a hospital bed.
So maybe keep the poetry for the blog and the Valsalva for the living.
Let’s get moving, friends! 🚀 Incorporate 10‑minute yoga or meditation into your morning routine and watch the stress‑hormone surge melt away, giving your heart a smoother ride.
/p>Pair that with a balanced diet rich in omega‑3s and you’ve got a recipe for rhythm stability. 🌟
Great tips! I’ve started a quick breathing session before bed and already notice fewer night‑time spikes. Thanks for the practical advice.
/p>When you’re navigating the ups and downs of SVT, think of yourself as an apprentice athlete training for a marathon, not a sprinter chasing instant glory.
/p>Each day you make a small adjustment – whether it’s swapping that second espresso for water, adding a brief walk after lunch, or scheduling that overdue cardiology check‑up – you’re laying a brick in the foundation of lasting health.
Consistency beats intensity; a steady, manageable routine will outlast occasional bursts of effort.
Remember to celebrate the tiny victories – a night without palpitations, a week of reduced caffeine, a successful Valsalva that restored calm.
These moments build confidence, which in turn reduces anxiety‑driven spikes.
Keep a simple journal: date, trigger exposure, heart rate, and how you felt.
Over weeks, patterns emerge, and you gain the insight to preempt episodes before they flare.
Most importantly, be kind to yourself; setbacks happen, but they do not define your journey.
Trust the process, stay persistent, and your heart will thank you.
Well said keep it simple focus on daily habits and you’ll see progress over time
/p>Listen up, the heart doesn’t care about your excuses or your Saturday night binge; it demands respect and disciplined care.
/p>Stop treating SVT like a mere inconvenience and start treating it like a warning siren that you’ve ignored for far too long.
Cut the caffeine, curb the alcohol, and stop letting stress run the show – you’re the commander of your own rhythm.
If you think medication is a crutch, remember that even the most powerful drugs can’t fix a lifestyle that constantly provokes the arrhythmia.
Embrace the vagal maneuvers, schedule regular check‑ups, and stop relying on luck to keep the beats in check.
Your heart will reward the effort with steadier pulses and fewer frantic episodes.
Sure, because the “big pharma” conspiracy is obviously hiding the real cure: a secret diet only the elite know about.
/p>In reality, the science is out there and the real secret is consistency, not hidden agendas.
Esteemed readers, it is incumbent upon us to acknowledge the paramount importance of evidence‑based interventions in the management of supraventricular tachycardia.
/p>Rigorous adherence to guideline‑directed therapy, encompassing both pharmacologic agents such as beta‑blockers and interventional procedures like catheter ablation, constitutes the cornerstone of optimal patient outcomes.
Moreover, diligent lifestyle modification, including the moderation of stimulants and the promotion of regular aerobic exercise, augments therapeutic efficacy.
Continuous monitoring and periodic reassessment are indispensable to ensure sustained rhythm stability.
In sum, a multidisciplinary approach, anchored in clinical rigor, offers the most favorable prognosis for affected individuals.
Thanks for the thorough rundown its helpful and makes the whole thing less scary
/p>