Treatment Effectiveness: How to Judge If a Therapy Works
When you're trying a new medication or therapy, how do you know it's actually working? A lot of people rely on hope or one-off changes. You should use clear, everyday checks that tell you if a treatment is helping or harming.
Start with goals. Ask what success looks like for you: less pain, lower blood pressure, fewer flare-ups, or better sleep. A clear goal lets you measure progress. If your goal is 'less pain,' pick a simple scale from 0 to 10 and score it before and after treatment.
Quick checks: what to look for
Track measurable signs. For blood pressure meds, use home readings. For diabetes drugs, watch A1c or fasting glucose. For infections, note fever, swelling, or wound healing. Simple numbers and symptoms tell you more than vague feelings.
Watch timing. Most treatments have a typical window to show effect. Antibiotics often work in 48–72 hours. Antidepressants can take weeks. If a therapy hasn’t shown expected change in the usual time, talk to your provider.
Side effects matter. Sometimes a drug seems to work but causes new problems. Keep a short daily log of side effects and how they affect daily life. If side effects outweigh benefits, your plan needs rethinking.
Monitoring and adjusting treatment
Use tests wisely. Lab tests, imaging, and validated scales help confirm results. Don’t ask for tests just to worry—ask for ones that will change the plan. For example, repeat A1c after three months if you started a diabetes med.
Be honest with your doctor. Tell them if you missed doses, stopped early, or used other remedies. Missing pills or mixing treatments changes effectiveness and can cause harm.
Consider real-world factors. Sleep, diet, stress, and exercise all affect outcomes. A blood pressure pill won’t fix a high-salt diet. Think of medication as one part of the plan, not a magic fix.
When to seek a second opinion. If progress stalls, side effects are severe, or you don’t trust the plan, a second professional view helps. A fresh look can spot interactions, alternative drugs, or non-drug options like therapy or physical rehab.
Compare options. Some conditions have many effective treatments. Ask which option is fastest, safest, cheapest, or easiest to stick with. If cost or access is a problem, ask about generics, alternative dosing, or patient programs.
Finally, keep records. A simple notebook or phone app with dates, doses, symptoms, and test results tells the full story. When you and your provider review clear data, decisions become easier and safer.
Watch for red flags: sudden worsening, strange new symptoms, allergic reactions, or signs of organ problems like dark urine or yellow skin. If your breathing gets worse, you get chest pain, fainting, or severe rash, seek care now. Also check interactions: herbal supplements, over-the-counter pain relievers, and alcohol change drug effects. Keep an updated med list and share it before any new prescription. Small warnings saved early can prevent big problems later.
Track, ask, adjust, repeat.
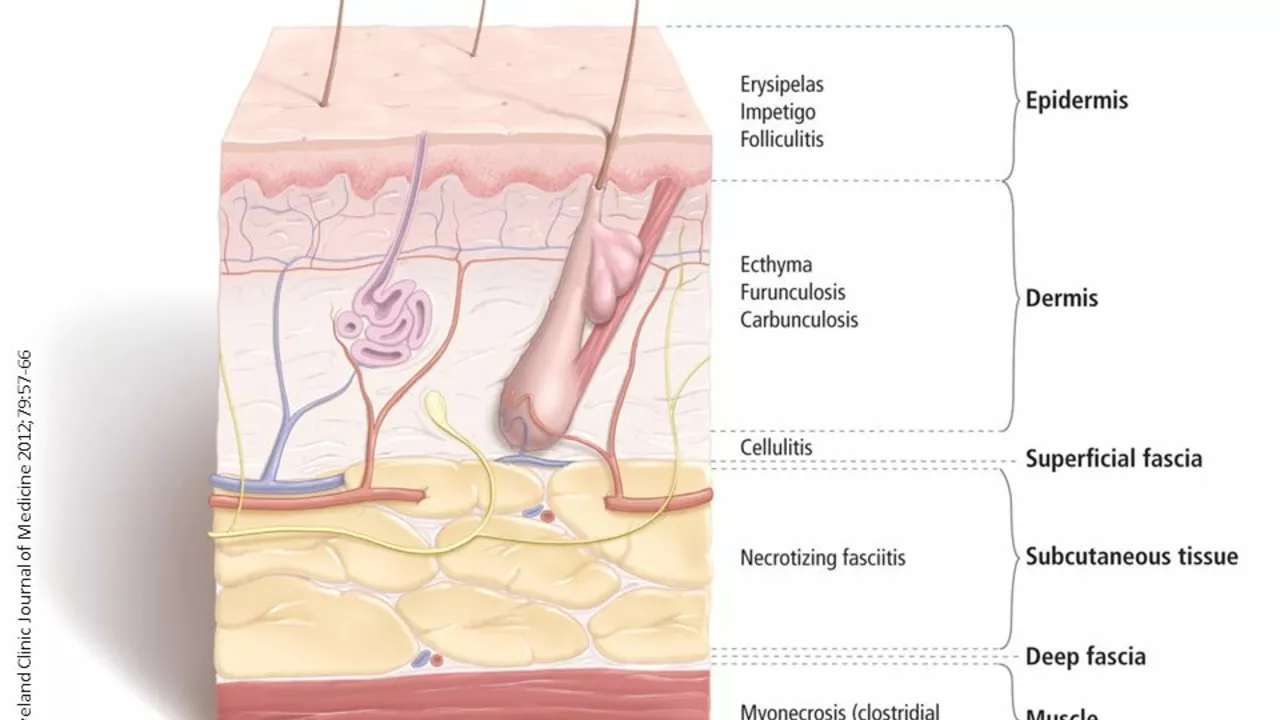
The Effectiveness of Fosfomycin in Treating Skin and Soft Tissue Infections
After researching, I've discovered that Fosfomycin is a highly effective antibiotic in treating skin and soft tissue infections. It's particularly potent against bacteria resistant to other antibiotics, which makes it a valuable option for tough infections. The drug works by interfering with the bacteria's ability to produce essential proteins, thus stopping their growth. Side effects are minimal, with gastrointestinal discomfort being the most common. All in all, Fosfomycin seems to be an excellent choice for tackling stubborn skin and tissue infections.