Understanding Teriflunomide and Its Effects on Liver Function
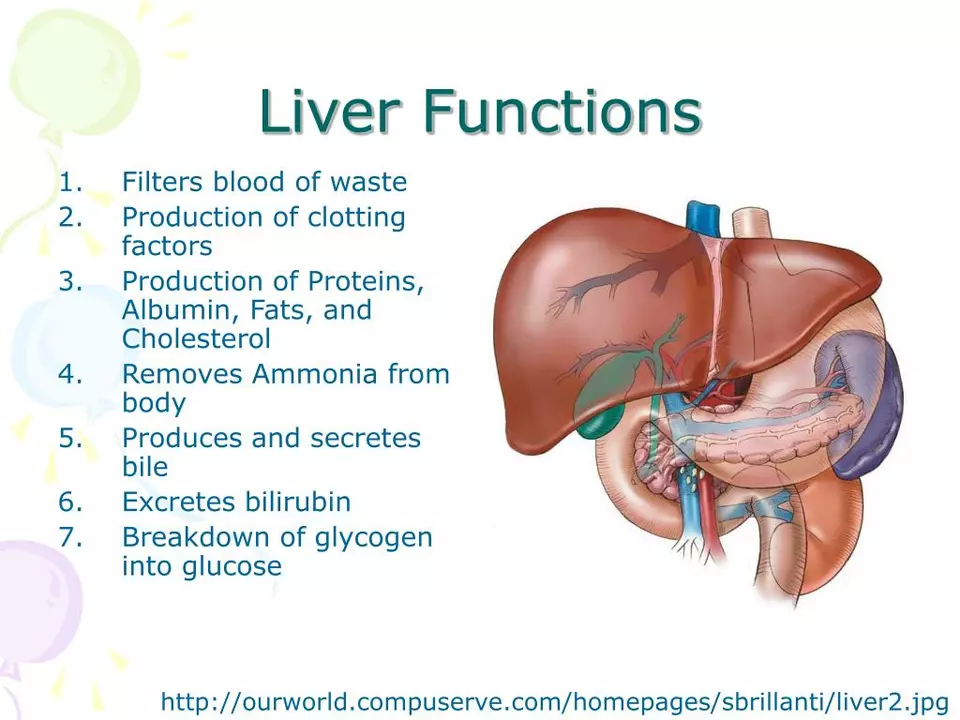
Teriflunomide is a medication commonly prescribed to manage the symptoms of multiple sclerosis (MS), a chronic, inflammatory disease that affects the central nervous system. It works by reducing inflammation and preventing the immune system from attacking the protective covering of nerve fibers. However, it is crucial to understand how this drug affects liver function and the potential risks it may pose to our overall health. In this section, we will explore the basics of teriflunomide and how it impacts liver function, setting the foundation for understanding the importance of monitoring and managing these risks.
Identifying the Potential Risks of Teriflunomide on Liver Function
One of the potential risks associated with teriflunomide use is its impact on liver function. Although it is generally well-tolerated, some patients may experience elevated liver enzymes, which can indicate potential liver damage. It is essential to be aware of the warning signs and symptoms of liver problems, such as jaundice (yellowing of the skin and eyes), dark urine, persistent nausea or vomiting, fatigue, and abdominal pain. If you experience any of these symptoms, it is crucial to consult your healthcare provider immediately to discuss your concerns and determine the appropriate course of action.
Monitoring Liver Function While Taking Teriflunomide
Given the potential risks associated with teriflunomide and liver function, regular monitoring is essential for ensuring your safety and the effectiveness of the medication. Your healthcare provider will likely perform routine blood tests to check your liver function before starting teriflunomide treatment and periodically throughout the course of treatment. These tests measure the levels of liver enzymes in your blood, which can indicate potential liver damage. By monitoring your liver function, your healthcare provider can identify any potential issues early on and take the necessary steps to manage your overall health.
Managing Risks and Maintaining Liver Health While on Teriflunomide
There are several steps you can take to maintain liver health and minimize the potential risks associated with teriflunomide treatment. First and foremost, it is essential to follow your healthcare provider's recommendations regarding the dosage and frequency of your medication. Additionally, maintaining a healthy lifestyle, including a balanced diet, regular exercise, and sufficient sleep, can help support liver function and overall health. Limiting alcohol consumption and avoiding other medications that may be harmful to the liver can also help reduce the potential risks associated with teriflunomide. If you have any concerns about your liver health, be sure to discuss them with your healthcare provider, who can provide guidance on managing these risks effectively.
When to Seek Medical Help and Possible Alternatives to Teriflunomide
If you experience any signs or symptoms of liver problems while taking teriflunomide, it is crucial to seek medical help immediately. Your healthcare provider may need to adjust your medication, perform additional tests, or recommend alternative treatments to manage your MS symptoms while protecting your liver health. There are several other medications available for treating MS, and your healthcare provider can help you determine which option is best for you based on your individual needs and any potential risks. Remember, the key to managing your health while on teriflunomide is open communication with your healthcare provider and staying proactive in monitoring and managing any potential risks.





15 Comments
Thanks for the thorough overview. It's good to know that regular liver function tests can catch any issues early, and staying hydrated helps too. I try to pair my meds with a diet rich in leafy greens and lean protein.
/p>Honestly, the liver warnings feel overblown-most patients breeze through without a hitch.
/p>i dunno why everyone makes a big drama about teriflunomide 😒 its just a pill, u get liver tests lol, just chill and dont overthink it 🙃
/p>While it's true the tests are routine, it's still wise to keep an eye on any odd symptoms. Even subtle fatigue can hint at something, so staying proactive never hurts.
/p>Excellent points!! Remember, consistent monitoring-every 3‑4 months-can significantly reduce risk!! Also, limit alcohol intake; the liver will thank you!!
/p>yeah good advice just remember to talk to your doc
/p>Hey folks! Just wanted to add that staying active-like a quick walk or yoga-can actually support liver health while you're on teriflunomide. It’s a simple habit that makes a big difference.
/p>The whole monitoring protocol feels like an overengineered safety net, but if it keeps the hepatocytes safe, who’s complaining.
/p>Jenny, you’ve got a point-regular LFTs are essentially a low‑cost sentinel system. They catch asymptomatic elevations early, which lets us tweak dosage before any serious hepatotoxicity develops.
/p>When it comes to teriflunomide, the conversation often polarizes between the fervent defenders of its efficacy and the alarmists who magnify every lab anomaly. I find myself straddling that line, contemplating both the molecular mechanisms and the lived experiences of patients. Teriflunomide’s inhibition of dihydroorotate dehydrogenase curtails pyrimidine synthesis, a pathway intimately tied to lymphocyte proliferation; that’s the therapeutic backbone. Yet, the liver, a central hub for metabolism, bears the brunt of many xenobiotics, and any perturbation can ripple through homeostasis. Elevated transaminases, while frequently transient, serve as biomarkers of hepatic stress, prompting a cascade of clinical decisions. Some clinicians adopt a watchful‑waiting approach, rechecking labs in two weeks, whereas others opt for an immediate dose reduction or even drug discontinuation. The latter strategy hinges on the principle of “first, do no harm,” but it also risks compromising disease‑modifying benefits for MS. Conversely, tolerating mild elevations might allow disease control to continue while the liver recalibrates. Lifestyle factors, such as alcohol consumption and concomitant hepatotoxic meds, modulate this risk spectrum, underscoring the need for a holistic assessment. Moreover, the availability of accelerated elimination procedures-like cholestyramine or activated charcoal-adds an extra safety valve for those who develop significant hepatotoxicity. Patient education becomes paramount; individuals should recognize subtle signs-fatigue, right‑upper‑quadrant discomfort, jaundice-and report them promptly. Ultimately, the therapeutic calculus is a dance between efficacy and safety, informed by vigilant monitoring and shared decision‑making. By embracing both the biochemical nuance and the human element, we can navigate the teriflunomide landscape with confidence and compassion.
/p>I appreciate the balanced view here. Emphasizing regular blood work while also encouraging a balanced diet seems like the sweet spot for many patients.
/p>While the article is informative; it lacks citations; ensure that future posts reference clinical guidelines!!
/p>i think the whole liver monitoring hype is just pharma scare tacts, most people never have real issues.
/p>Actually, the data clearly shows teriflunomide rarely causes severe hepatotoxicity.
/p>Dear Patrick, while recent studies do indicate a low incidence of serious liver injury, it remains prudent to adhere to established monitoring protocols to safeguard patient welfare.
/p>