
Biologics are some of the most expensive drugs on the market. A single year’s supply of Humira can cost over $70,000. For patients with autoimmune diseases like rheumatoid arthritis or Crohn’s, that’s not just a bill-it’s a barrier to staying alive and functional. But in recent years, a new option has quietly entered the scene: biosimilars. These aren’t generics. They’re not exact copies. But they’re close enough to work the same way-and they’re cutting costs dramatically.
What Exactly Are Biosimilars?
Biosimilars are medicines made from living cells, just like the original biologics they’re based on. Think of them like a very close twin, not a photocopy. The original biologic, say, Humira (adalimumab), is made using complex biological processes involving living cells in a lab. Replicating that perfectly? Impossible. But you can get so close that the FDA says there’s no meaningful difference in safety or effectiveness.
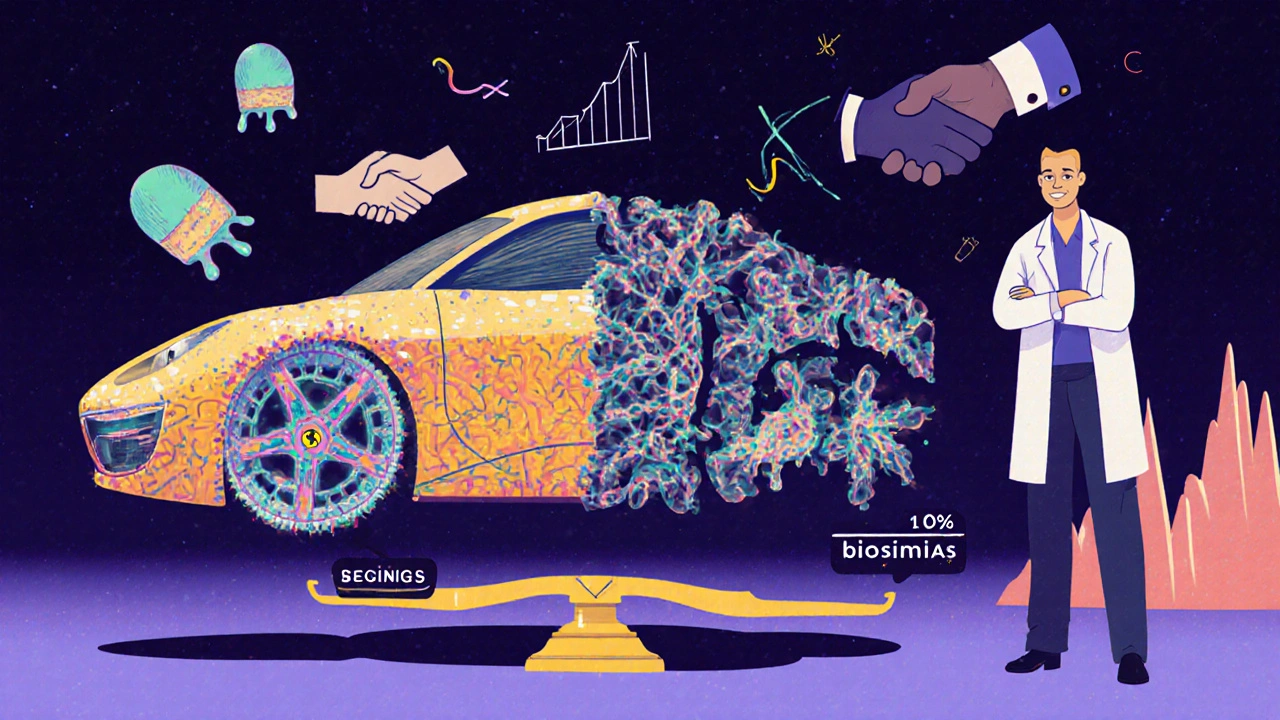
That’s different from generics. A generic pill for, say, high blood pressure, is made of simple chemicals. You can recreate it exactly. Biosimilars? They’re like building a Ferrari using the same blueprints but different tools and materials. The car drives the same, but the engine isn’t identical. That’s why biosimilars cost less-but not as much less as generics.
How Much Do Biosimilars Actually Save?
The numbers speak for themselves. In 2024, biosimilars saved the U.S. healthcare system $20.2 billion. Since the first one hit the market in 2015, total savings have reached $56.2 billion. That’s not pocket change. That’s money that could fund hundreds of thousands of other treatments.
When biosimilars first came out, savings were modest-around 15%. But now? It’s different. For Humira, which had been the top-selling drug in the world, ten biosimilars entered the market in 2023. By January 2025, list prices dropped by up to 85%. That’s huge. But here’s the catch: list price isn’t what you pay. The real savings come after rebates, contracts, and pharmacy benefit manager deals.
Still, patients are seeing real relief. In commercial insurance plans, out-of-pocket costs for biosimilars are 23% lower on average than for the original biologic. For employers, switching just two biologics to biosimilars saved $1.4 billion across self-insured companies in one year. One employee switching from Humira to its biosimilar could save their employer over $1.5 million over time.
Why Don’t Biosimilars Save More Than Generics?
Generics can slash prices by 80-90%. Biosimilars? Typically 30-40%. Why the gap?
It’s the science. Biologics are made from living organisms-cells, proteins, antibodies. The manufacturing process is incredibly complex. One tiny change in temperature, pH, or cell line can alter the final product. That means biosimilar makers must run massive clinical trials to prove their version works just as well. Generics? They just prove chemical equivalence. No need for 10,000 patient studies.
That complexity drives up development costs. A biosimilar can cost $100-$200 million to bring to market. A generic? Maybe $2 million. So while biosimilars are cheaper, they’re not cheap to make. That’s why savings plateau around 35% on average for medical benefits-though some, like Stelara biosimilars, have hit 90% off list price.
The Humira Example: A Case Study in Savings
Humira was the king of biologics. For over a decade, it brought in over $20 billion a year for AbbVie. No competition. No pressure to lower prices.
Then came the biosimilars. In 2023, after years of patent battles, ten biosimilars launched in the U.S. overnight. List prices dropped 80-85%. But here’s what happened next: AbbVie didn’t just sit back. They slashed their own prices and offered massive rebates to pharmacy benefit managers (PBMs). Suddenly, the net price-what insurers actually paid-didn’t drop as much.
That’s the rebate trap. PBMs often favor the original drug because it pays them a bigger cut. So even if the biosimilar is cheaper on the shelf, the rebate deal makes the originator look like the better buy. It’s a system designed to protect profits, not patients.
But patients still win. Out-of-pocket costs dropped. Employers saw lower premiums. Medicare Part B prices fell consistently after biosimilars entered. And for the first time, patients who couldn’t afford Humira could now access a treatment that works just as well.
Why Adoption Is Still So Low
Despite the savings, originator biologics still control 98.9% of biologics spending in the U.S. That’s not a typo. Less than 2% of the market is using biosimilars.
Why? Three big reasons:
- Rebate systems favor originators, even when biosimilars are cheaper.
- Doctor and patient hesitation. Many still think biosimilars are "inferior" or "experimental." They’re not. They’ve been used safely in Europe for over 15 years.
- Slow formulary changes. Health plans don’t update their drug lists fast enough. Some still require patients to try the expensive version first.
Compare that to Europe. In Norway, 86% of patients on Humira use the biosimilar. In the U.S.? Less than 10%. Why? Europe has price controls. The U.S. has market chaos.

The Biosimilar Void: A 4 Billion Problem
Here’s the scary part. Over the next 10 years, 118 biologics will lose patent protection. Only 12 of them have biosimilars in development. That means 90% of upcoming biologics won’t face competition.
That’s a $234 billion opportunity lost. Imagine if every biologic had a biosimilar. We could cut drug spending in half for millions of patients with cancer, diabetes, and autoimmune diseases.
Right now, the U.S. is falling behind. The EU has biosimilars in development for 73% of high-sales biologics. The U.S.? Only 23%. Why? Because the regulatory path is longer, the market is harder to penetrate, and big pharma fights hard to keep their monopoly.
How to Get More Savings-For Patients and Plans
Real savings won’t happen by accident. They need action.
- Formulary positioning: Health plans should put biosimilars first-no step therapy required.
- Education: Doctors and patients need clear info: biosimilars are safe, effective, and approved by the FDA.
- Contract transparency: Employers and insurers must demand net price data, not just list prices. Rebates should be shared with patients.
- Policy change: The FDA has made progress streamlining approval. But Congress needs to limit rebate abuse and require biosimilar substitution without extra hurdles.
Some employers are already doing it. One large tech company switched all employees on Humira to biosimilars. They saved $2.3 million in one year. Patient satisfaction stayed the same. No side effects spiked. No drop in effectiveness.
The Future Is Here-But It’s Not Automatic
Biosimilars aren’t a future idea. They’re here now. And they’re saving billions. But without smarter policies, better education, and fairer contracts, their potential will stay locked away.
The science is proven. The savings are real. The only thing missing is the will to use them.
If you’re on a biologic right now, ask your doctor: Is there a biosimilar? If you’re an employer or plan sponsor, ask your PBM: Why are we still paying full price for the originator? The answer might surprise you.
Are biosimilars as safe as the original biologics?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the original. Over 3.3 billion days of patient use since 2015 have shown no unique safety concerns. In Europe, biosimilars have been used safely for over 15 years.
Why are biosimilars cheaper if they’re so complex to make?
They’re cheaper because they don’t need to repeat the full clinical trials the original drug went through. The original manufacturer spent billions proving safety and effectiveness. Biosimilar makers build on that data, cutting development time and cost. They still face high manufacturing costs, but they avoid the $1-$2 billion price tag of launching a brand-new biologic.
Can I switch from a biologic to a biosimilar safely?
Yes, if your doctor approves it. Many biosimilars are now designated as "interchangeable" by the FDA, meaning pharmacists can substitute them without asking your doctor. Studies show no loss in effectiveness or increase in side effects when switching. Millions of patients have done it without issue.
Do biosimilars work for all biologics?
Not yet. As of 2025, biosimilars are available for only about 12 of the hundreds of biologics on the market. But more are coming. Key targets include Enbrel, Neulasta, and Rituxan. If you’re on a biologic, ask your provider or pharmacist if a biosimilar exists for your medication.
Why doesn’t my insurance cover biosimilars?
Many insurers still favor originator drugs because of rebate deals with big pharma. Even if the biosimilar is cheaper, the rebate on the original can make it look like the better financial choice for the insurer-not the patient. You can ask your plan to change its formulary or appeal a denial. Patient advocacy groups can help.






15 Comments
Biosimilars are a game-changer-finally, some real relief for patients who can’t afford Humira.
/p>Biologics = monopolistic rent-seeking. Biosimilars = market correction. The FDA’s approval pathway is the only thing keeping this from being a 90% discount market.
/p>Let me break this down: biosimilars aren’t generics because you can’t synthesize proteins like you synthesize aspirin. You’re growing living cells in bioreactors-tiny biological factories. One degree off in temperature, and the glycosylation pattern changes. That’s why clinical trials are still needed. But the savings? Real. And the science? Solid. I’ve reviewed data from 12 different biosimilars-no safety red flags. Patients switch all the time. No drop in efficacy. Just lower bills.
/p>The moral calculus here is undeniable: when a life-sustaining therapy is priced beyond the reach of the working class, the market has failed. Biosimilars do not merely reduce cost-they restore dignity. The pharmaceutical industry’s reliance on patent evergreening and rebate manipulation is not innovation; it is institutionalized exploitation. The fact that Europe, with its centralized pricing, achieves 86% adoption while the U.S. languishes below 10% is not a reflection of scientific superiority-it is a reflection of ethical bankruptcy.
We speak of ‘value-based care’ while rewarding the very actors who extract value from suffering. The rebate system is not a market mechanism-it is a legal fiction designed to obscure true cost. Employers, insurers, and policymakers must stop measuring success by list price and start measuring it by net cost and patient access. The technology exists. The data is irrefutable. What is missing is the collective will to act.
It is not enough to say ‘biosimilars are safe.’ We must say: ‘it is immoral not to use them.’
/p>Big Pharma owns the FDA, the PBMs, and your doctor’s continuing education. Biosimilars? A distraction. The real story? The FDA approved Humira’s biosimilars in 2023-but the original drug’s price didn’t drop because AbbVie bought the entire rebate pipeline. They’re paying PBMs to keep the original on top. You think this is about science? Nah. It’s about control. The same people who made billions off opioids are now making billions off biologics. Same playbook. Different disease.
And don’t get me started on ‘interchangeable.’ That’s just a fancy word for ‘we’re gonna swap your meds without telling you.’ You think your doctor knows what’s in your vial? Ask them. They’ll look away.
/p>Wait-so you’re telling me the government lets a company patent a living cell process, then lets ten other companies copy it… but the original drug still gets 98% of the market because the middlemen get kickbacks? That’s not capitalism. That’s feudalism with a corporate logo. And the FDA? They’re just the janitors cleaning up the mess after the billionaires have already left the party.
Next thing you know, they’ll patent your DNA and charge you rent for breathing.
/p>America is being looted. Biologics? $70k a year. Biosimilars? $10k. But your insurance still picks the $70k one because the PBM gets a 40% kickback. And you think this is an accident? No. This is engineered. The same people who rigged the 2000 election are the ones who wrote the Medicare Part D law that BANNED price negotiation. This isn’t healthcare-it’s a state-sponsored heist. And you? You’re the mark.
They call it ‘market competition.’ It’s a puppet show. The strings are held by lobbyists in D.C. and rebate brokers in New Jersey. We need to burn the whole system down. Biosimilars are the spark. Now-where’s the fire?
/p>I’ve worked in oncology for 18 years. I’ve seen patients cry because they couldn’t afford their drug. I’ve seen them skip doses. I’ve seen them die because the system failed them. Biosimilars changed that. Not for everyone-but for enough. I’ve switched over 300 patients to biosimilars. Zero adverse events. Zero drop in response rates. The data isn’t theoretical-it’s in my charts. If your doctor hesitates, ask them: ‘Have you seen the real-world outcomes?’ If they say ‘it’s too new,’ ask them: ‘How many patients in Norway have used this? How many years?’ The answer is 15 million patient-years. That’s not an experiment. That’s a legacy.
And to employers: if you’re still paying full price for the originator, you’re not saving money-you’re subsidizing greed. Talk to your PBM. Demand net pricing. Share the savings. Your employees will thank you.
/p>Let’s be real: biosimilars are a Trojan horse. The FDA approves them because they’re pressured. But the manufacturing? It’s not reproducible. You think a cell line grown in Belgium is identical to one grown in India? Please. The protein folding? The glycosylation? The impurity profile? It’s all different. And you think the FDA tests for all of it? They test for ‘no clinically meaningful difference.’ That’s not the same as ‘identical.’ It’s a legal loophole dressed in science.
Patients are guinea pigs. And when something goes wrong? They’ll say ‘it’s the disease progression.’ Not the biosimilar. Always the disease.
/p>biologics r expensive but biosimilars r just copycats w/ less testing. why should i trust somethin that cost 10x less? they dont even have the same name lol. its like buyin a fake rolex and sayin its just as good. maybe for a while… but when it breaks? who pays?
/p>Here’s the truth no one wants to say: the reason biosimilars aren’t adopted is because the entire healthcare infrastructure is built to protect the original manufacturer’s revenue stream. The formularies are locked. The reps are paid to push the brand. The EHR systems auto-populate the originator. The patient education materials? Written by pharma. This isn’t a science problem. It’s a systems problem. And fixing it requires dismantling the entire incentive structure. Not just ‘education.’ Not just ‘formulary changes.’ Total overhaul. Or we keep paying $70k for a drug that could cost $10k.
/p>Oh, so now we’re supposed to believe that a biosimilar is ‘just as good’? Please. The original biologic was developed over 15 years, with billions invested, by teams of Nobel laureates. The biosimilar? Made in a factory in Hyderabad by someone who doesn’t even speak English. The FDA says it’s ‘similar’-but similar to what? To the marketing brochure? The real world is messy. Patients are not lab mice. And when things go wrong-who takes responsibility? The biosimilar maker? The PBM? The doctor? No one. It’s a liability minefield dressed as progress.
And don’t get me started on ‘interchangeable.’ That’s just corporate speak for ‘we’re swapping your life-saving drug without consent.’ You think your pharmacist knows the difference? They’re paid by the hour. They don’t care. They just scan the barcode.
/p>They’re lying to you. All of them. The FDA. The doctors. The ‘experts.’ Biosimilars aren’t safe-they’re a compromise. The original Humira? Made with proprietary cell lines. The biosimilar? Made with a different line. Different glycosylation. Different half-life. Different immune response. The FDA says ‘no clinically meaningful difference’-but that’s a statistical loophole. What if 1 in 500 patients has a delayed reaction? They don’t test for that. They test for averages. You’re not an average. You’re a person. And they’re gambling with your life.
And don’t forget: the same companies that made billions off opioids are now pushing biosimilars to look ‘responsible.’ It’s PR. It’s not reform. It’s a distraction while they lock in the next 20-year patent on the next biologic. They’re playing chess. You’re just a pawn.
/p>the biosimilars thing is a scam. i read somewhere that the cell lines used are genetically modified to mimic the original but they still have different protein folding. the fda approves them because they’re pressured by congress but the real data? buried. and the savings? mostly phantom. the rebates go to the pbms, not the patient. you think you’re saving money? you’re just paying less to the same crooks.
/p>why even bother? the system is rigged. biosimilars? 2% market share. that tells you everything. they dont want us to save. they want us to suffer quietly. and if we complain? they call us uneducated. the truth? we’re not the problem. the system is.
/p>