
Steroid Cataract Risk Calculator
This tool helps you understand your personal risk of developing steroid-induced cataracts based on your treatment factors. Regular eye exams are essential for early detection.
When you're on long-term steroids for asthma, rheumatoid arthritis, or a skin condition, you’re probably focused on managing the disease - not your eyes. But here’s something most people don’t realize: steroid-induced cataracts can develop faster than you think, and they can turn everyday tasks like reading, driving at night, or recognizing faces into a struggle. Unlike age-related cataracts that creep in over decades, these can show up in as little as two months. And if you’re using steroid eye drops, inhalers, or pills, you’re at risk.
How Steroids Damage Your Lens
Steroid-induced cataracts aren’t just cloudy lenses. They’re a specific type called posterior subcapsular cataracts (PSCs). These form right at the back of the lens, where light enters. That’s why even a tiny opacity can wreck your vision. While regular cataracts blur your sight slowly, PSCs hit hard and fast - especially with glare, reading, and night vision. The science behind it is complex, but the bottom line is this: steroids interfere with the proteins inside your lens. Normally, these proteins stay clear and organized. Steroids cause them to clump together like scrambled eggs. This clumping scatters light before it reaches your retina, creating haze, halos, and ghost images. Research shows these changes happen because steroid molecules bond with lens proteins in a way that’s unique to corticosteroids - no other type of cataract shows this exact pattern. On top of that, steroids lower your eye’s natural defenses. Your lens relies on antioxidants to fight off damage from daily exposure to light and oxygen. Steroids reduce those antioxidants, letting free radicals build up and wreck more protein structure. The lens can’t repair itself - it has no blood supply - so once the damage starts, it only gets worse.What You’ll Notice: The Real Symptoms
If you’re on steroids and your vision feels off, don’t brush it off as “just tired eyes.” These are the signs that show up in over 75% of cases:- Blurry vision - especially up close. Reading the menu or your phone screen becomes a chore.
- Glare and halos - headlights at night look like starbursts. Bright sunlight feels blinding.
- Faded colors - reds look dull, whites look yellowish. You might say, “Everything looks washed out.”
- Double vision - even with one eye closed.
- Difficulty seeing at night - driving after dark becomes risky.
- Reduced peripheral vision - you miss things out of the corner of your eye.
Who’s Most at Risk?
It’s not just about how much steroid you take - it’s how long, how often, and how you take it.- Topical steroids - eye drops, creams, or nasal sprays - carry the highest risk. Studies show they’re 3.2 times more likely to cause cataracts than oral or inhaled forms.
- Duration - 4 months or more of continuous use raises the risk sharply. But some people see changes in as little as 2-4 weeks.
- Dose - taking more than 2,000mg of beclomethasone (a common inhaled steroid) significantly increases your odds.
- Age - children and older adults are more vulnerable. Kids on long-term steroids for eczema or autoimmune disorders often develop cataracts early.
- Other conditions - if you have diabetes, uveitis, or already have an artificial lens (IOL), your risk multiplies.

How Doctors Spot It Early
The key to avoiding major vision loss is catching it before it’s too late. That’s why regular eye exams aren’t optional - they’re essential. Before you start long-term steroid treatment (defined as more than two weeks), you should get a baseline eye exam. After that, follow-up exams every 3-6 months are recommended if you’re on high doses or have other risk factors. Ophthalmologists use a tool called a slit-lamp - a powerful microscope with a bright light - to look deep into your lens. They’re trained to spot the earliest signs of PSCs: a faint, granular haze right behind the lens capsule. These changes can appear months before you notice any symptoms. In fact, residents in eye training programs take 6-12 months of supervised practice to reliably identify these early signs. It’s easy to mistake steroid-induced cataracts for age-related ones, especially in older patients. But PSCs have a distinct shape and location. If your doctor doesn’t check for them specifically, they might miss it.Treatment: Surgery Is the Only Fix
There’s no pill, drop, or supplement that can reverse steroid-induced cataracts. Once the lens proteins are clumped, they don’t unclump. The only proven treatment is cataract surgery. The procedure is routine: the cloudy natural lens is removed and replaced with a clear artificial one (an IOL). Success rates are high - 92% of patients report major vision improvement after surgery. Colors come back. Glare fades. Night driving becomes possible again. But here’s the hard part: if you still need steroids after surgery, your new lens isn’t immune. The same protein damage can happen again. That’s why doctors monitor you closely after surgery. Some patients need repeat procedures or extra treatments to manage ongoing inflammation. Before surgery, your doctor might try to reduce your steroid dose - but only if your main condition allows it. Stopping steroids suddenly can cause serious flare-ups. For someone with lupus or severe asthma, the risk of stopping may be worse than the risk of vision loss. That’s why decisions must be made together - with your rheumatologist, pulmonologist, or dermatologist, and your eye doctor.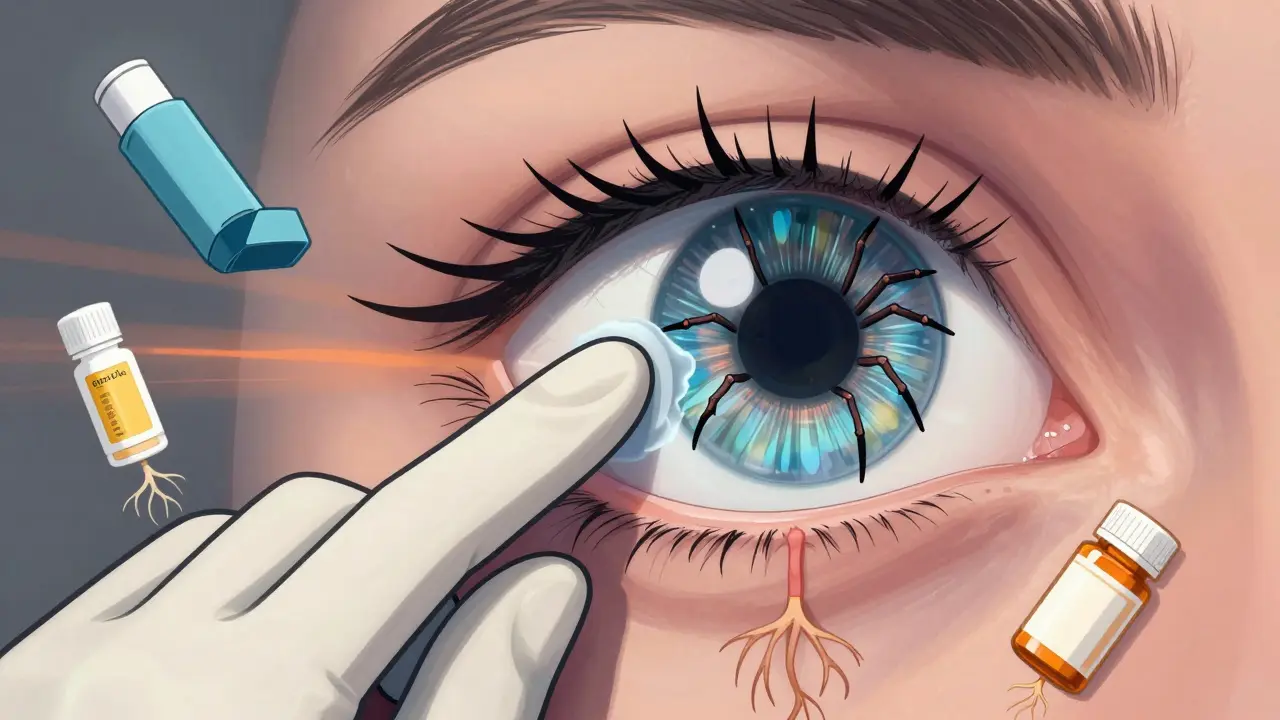
Can You Prevent It?
Prevention isn’t about avoiding steroids when you need them. It’s about minimizing damage while using them.- Use the lowest effective dose - always. Don’t increase it without medical advice.
- Limit duration - ask if you can taper off sooner than planned.
- Choose the right form - if possible, avoid steroid eye drops unless absolutely necessary. Inhaled steroids are safer for your eyes than drops.
- Protect your eyes - wear UV-blocking sunglasses. Sunlight increases oxidative stress, which steroids already weaken.
- Get checked regularly - every 6 months if you’re on long-term therapy. Don’t wait for symptoms.
What Happens If You Ignore It?
Left untreated, steroid-induced cataracts don’t just blur your vision - they can lead to permanent disability. You might lose your driver’s license. You could fall more often. You might stop reading, socializing, or doing the things you love. Worse, cataracts can hide other steroid-related eye problems - like glaucoma. High eye pressure from steroids can damage your optic nerve. And once that nerve is damaged, it doesn’t heal. So when you finally go to the eye doctor for blurry vision, you might discover two problems: one you can fix (the cataract), and one you can’t (the nerve damage).Final Thoughts
Steroid-induced cataracts are a silent side effect. They don’t hurt. They don’t itch. They just steal your vision - quietly, quickly, and often without warning. If you’re on steroids, your eyes need as much attention as your lungs, joints, or skin. Don’t wait until you can’t read your child’s school email or drive to work. Schedule that eye exam. Ask your doctor: “Could my meds be affecting my vision?” The good news? If caught early, surgery can restore your sight. The better news? You can control your risk - by being informed, asking questions, and staying on top of your eye health.Can steroid eye drops cause cataracts?
Yes. Steroid eye drops are one of the most common causes of steroid-induced cataracts. Studies show they carry a 3.2 times higher risk than oral or inhaled steroids. Even short-term use - like a few weeks for an eye infection - can trigger changes in the lens. That’s why doctors limit how long you can use them and monitor eye pressure and lens clarity during treatment.
Are steroid-induced cataracts reversible without surgery?
No. Once the lens proteins have clumped due to steroid exposure, they can’t be undone by drops, supplements, or lifestyle changes. The only way to restore clear vision is through cataract surgery, where the damaged lens is removed and replaced with an artificial one. Stopping steroids may slow further damage, but it won’t reverse what’s already happened.
How long does it take for steroids to cause cataracts?
It varies. Some people develop early signs in as little as 2-4 weeks, especially with high-dose eye drops. For most, noticeable changes appear after 3-6 months of continuous use. By 4 months, the risk increases significantly. The longer and stronger the steroid exposure, the faster and more severe the cataract becomes.
Can children get steroid-induced cataracts?
Yes. Children on long-term steroid therapy - for conditions like nephrotic syndrome, eczema, or autoimmune diseases - are at high risk. Their lenses are still developing, making them more sensitive to steroid damage. Ocular hypertension and posterior subcapsular cataracts are well-documented side effects in pediatric patients. Regular eye exams are critical for any child on steroids for more than a few weeks.
Do I need to stop my steroids before cataract surgery?
Not necessarily. Stopping steroids can be dangerous if you rely on them to control a serious condition like asthma, lupus, or Crohn’s disease. Your surgeon and prescribing doctor will work together to balance your vision needs with your overall health. In many cases, surgery proceeds while you continue steroids, but you’ll need closer monitoring afterward because the artificial lens can still be affected.
How often should I get my eyes checked if I’m on steroids?
If you’re on long-term steroid therapy (more than 2 weeks), get a baseline eye exam before starting. After that, follow up every 3-6 months. If you’re on high doses, use steroid eye drops, or have diabetes or glaucoma, your doctor may recommend exams every 3 months. Don’t wait for symptoms - early detection is the best defense.


8 Comments
So let me get this straight - you're telling me my asthma inhaler is slowly turning my vision into a bad YouTube filter? Like I'm living in a TikTok filter where everything's blurry and glowing? I've been on this thing for 3 years and I thought I was just getting old. Turns out I'm basically a walking lab experiment for Big Pharma's secret cataract program. I'm not even mad, I'm just impressed. They got me good.
/p>OMG I KNEW IT!!! 😱 My mom died from cataracts and she was on prednisone for lupus. They never told us this was coming. Now I'm scared to even breathe near a steroid cream. I think the government is hiding this. Why else would they let doctors keep prescribing it? It's like they want us blind so we don't see what's really going on. 😭
/p>This is such an important post. I work with diabetic patients on long-term steroids and I see this happen all the time. Many don't realize the connection until it's too late. I always remind them: your eyes are part of your body too. A simple 10-minute eye exam every 6 months can save your independence. Please, if you're on steroids, don't wait for symptoms. Prevention is better than surgery. 🙏
/p>So you're telling me my 2000mg of beclomethasone is slowly frying my lens proteins? Cool. So what's the real cost? I mean, if I stop the steroid I die. If I keep it I go blind. That's not a choice, that's a trap. And who pays for the surgery? Not the insurance. Not the pharma company. Just me. And then they sell me new glasses and call it a day. This system is rigged.
/p>People need to stop blaming the medicine and start taking responsibility. If you're on steroids long term you're not a victim, you're making a choice. You chose to live with your disease over your vision. So don't cry when the consequences come. And if you're too lazy to get an eye exam every 6 months then you deserve what you get. Wake up. Your eyes aren't magic. They're tissue. And tissue breaks when abused.
/p>Thank you for writing this. I'm on inhaled steroids for asthma and I had no idea. I just thought my night driving was getting worse because I'm tired. But now I'm scheduling my eye exam next week. I'm so glad I found this. You're right - it's silent until it's not. Don't wait. Just go. Your future self will thank you. 💙
/p>Why are we even using steroids anyway? In the 80s we didn't need them. Now every kid with a sniffle gets a nasal spray. This is all about control. The government wants us dependent. The doctors want the prescriptions. The pharma companies want the profits. And we're the ones losing our vision. It's not science. It's a system. And it's designed to break us down slowly. Wake up.
/p>Okay but like... imagine your lens proteins are just vibing, minding their own business, then BAM - steroid molecules show up like a toxic ex and start clumping everything like a bad Tinder date. 🥴 It's not just cataracts, it's emotional trauma for your eyeballs. I need a therapist AND an ophthalmologist now. 😭✨
/p>