Medication Monitoring: Simple Checks to Stay Safe
Taking medicine works best when you keep an eye on how it affects you. Monitoring is about simple checks, tests, and notes that help catch problems early. You don’t need medical training to do most of it—just a plan and honest reporting to your provider.
Start with a baseline
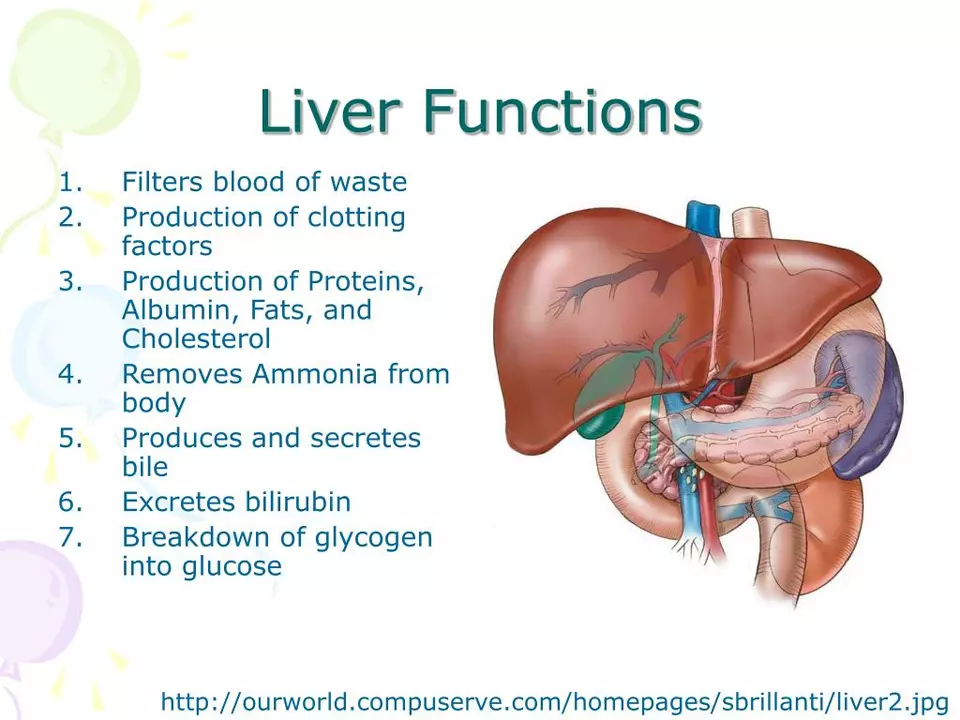
Before starting a new drug, ask your clinician for basic tests. For blood pressure drugs and ACE inhibitors like lisinopril check kidney function and potassium. For statins or combo drugs like Vytorin ask for liver tests and a lipid panel. If a medicine affects blood sugar, request fasting glucose or A1C. Baseline numbers make later changes easy to spot.
Do daily home checks
Do daily home checks. Measure blood pressure, pulse, weight, or blood sugar depending on your condition. Record each reading with date, time and any symptoms like dizziness, swelling, or lightheadedness. A short phone note, spreadsheet, or app screenshot works. Bring these notes to appointments so decisions are faster and safer.
Know common lab schedules. Many providers check kidney and electrolytes one to two weeks after starting ACE inhibitors or diuretics. Liver tests for statins are often rechecked at six to twelve weeks, especially if you have symptoms. For warfarin follow INR closely until stable; for direct oral anticoagulants check kidney function at least once a year. Drugs such as lithium, digoxin, phenytoin and valproate often require therapeutic drug monitoring by blood level.
Spot serious warning signs. Stop the drug and contact care if you get a sudden rash, trouble breathing, high fever, yellowing skin or eyes, severe stomach pain, fainting, rapid heartbeat, or sudden muscle weakness. Mild nausea or headache can be common early on, but any rapid worsening needs urgent review.
Keep a clear medication list. Note drug name, dose, why you take it, start date and prescriber. Include over-the-counter medicines, supplements and herbal products. Many interactions come from supplements people forget to mention.
Use at-home devices wisely. Buy validated blood pressure cuffs and calibrated glucometers. Follow user guides and clean devices. Send or show regular readings to your clinician before visits. Remote monitoring improves care when readings are accurate and shared.
Don’t stop or change doses without advice. If side effects bother you ask about dose adjustment or safer alternatives. Ask your clinician: what tests do I need, how often, what targets do we aim for, and when should I call? Clear answers make monitoring predictable and useful.
Special groups need closer checks. Older adults and people with kidney or liver disease often need more frequent labs and dose adjustments. Pregnant women require tailored monitoring for some drugs, and children may need weight-based dosing and extra follow-up. Mention allergies and past adverse reactions so clinicians can avoid repeats. If you travel, pack a list, medicine and contact info and ID.
Monitoring is teamwork. You provide daily checks and honest symptom notes. Your clinician orders the right labs and interprets trends. Together you catch problems early, tweak treatment, and keep therapy safe and effective.
Teriflunomide and Liver Function: Monitoring and Managing Risks
In today's blog post, we'll be discussing Teriflunomide and its effects on liver function. Teriflunomide is a drug used to treat multiple sclerosis, but it comes with some potential risks to our liver. It's essential to closely monitor liver function while taking this medication to manage and mitigate any possible side effects. We'll delve into the importance of regular liver function tests and explore some tips on maintaining a healthy liver while using Teriflunomide. Stay tuned for practical advice on ensuring your liver stays in top shape while benefiting from this treatment.