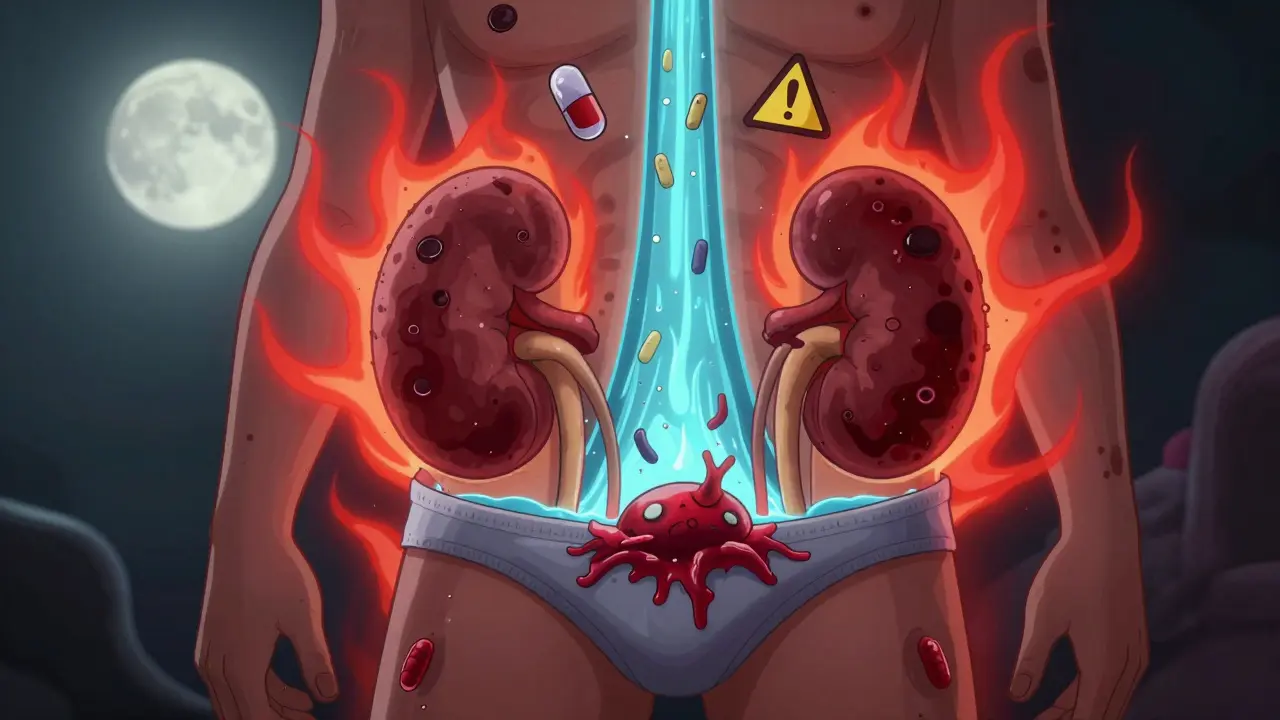
When you’re managing type 2 diabetes, taking an SGLT2 inhibitor like canagliflozin, a sodium-glucose cotransporter-2 inhibitor that lowers blood sugar by making the kidneys flush out excess glucose through urine, can be life-changing. These drugs reduce heart failure risk, protect kidney function, and help with weight loss. But there’s a rare, serious side effect you need to know about - Fournier’s gangrene, a fast-spreading, life-threatening infection that destroys skin and tissue around the genitals and anus. It’s uncommon, but when it happens, every hour counts.
What Exactly Is Fournier’s Gangrene?
Fournier’s gangrene isn’t just a bad infection. It’s a necrotizing fasciitis - a type of bacterial invasion that eats through layers of tissue, starting in the genital or perineal area. The bacteria, often a mix of E. coli, Staphylococcus, and anaerobes, spread rapidly through the fascia, cutting off blood supply. Skin turns black, swelling becomes severe, and the pain? Patients describe it as worse than childbirth or a broken bone. Fever, chills, and a feeling of extreme sickness usually follow.
It’s not new. The condition was first described in 1764. But in the last decade, doctors started seeing it pop up in people taking SGLT2 inhibitors. Between 2013 and 2018, the U.S. FDA confirmed 12 cases linked to these drugs. By 2024, the number had climbed. Most cases were in men - but about one-third were in women. That’s important. Many still think this only affects men. It doesn’t.
Why Do SGLT2 Inhibitors Increase the Risk?
The answer lies in how these drugs work. Dapagliflozin, empagliflozin, and the others all force your kidneys to dump glucose into your urine. That sounds good - it lowers blood sugar. But it also means your underwear becomes a sweet, moist breeding ground for bacteria.
Think of it like leaving sugar water in a warm, dark place. Bacteria thrive. In some people, especially those with poorly controlled diabetes, the immune system can’t keep up. The glucose in urine weakens local defenses. The skin around the genitals gets irritated. A small cut, a yeast infection, or even friction from tight clothes can become an entry point. Once the bacteria get in, they multiply fast, and the infection spreads deeper than you’d expect.
It’s not just glucose. High blood sugar itself damages nerves and blood vessels. That means people with diabetes often don’t feel the early pain. They might ignore redness or swelling, thinking it’s just a rash. By the time they feel real pain, it’s already too late.
Early Warning Signs You Can’t Ignore
Here’s what to watch for - and don’t wait. If you’re on an SGLT2 inhibitor and notice any of these, go to the ER immediately:
- Severe pain in the genitals, anus, or inner thighs - worse than a urinary tract infection
- Swelling or redness that spreads quickly - not just a small area
- Dark or discolored skin - purplish, black, or bruised-looking patches
- Fever above 38°C (100.4°F) or chills
- Foul-smelling discharge from the genital area
- General feeling of being extremely ill - like you’re about to pass out
These symptoms don’t show up slowly. They can go from mild discomfort to life-threatening in under 24 hours. One patient in a 2022 study went from noticing redness to needing emergency surgery in 14 hours. Another waited two days because he thought it was a yeast infection. He didn’t survive.

What Happens If You Ignore It?
Delay kills. Studies show that for every hour treatment is delayed, the risk of death rises by about 9%. If surgery is delayed beyond 24 hours, mortality jumps from 4% to over 25%. That’s not a small risk. That’s a death sentence.
Doctors have to cut away dead tissue - sometimes entire sections of skin, muscle, and even parts of the penis or scrotum. They give strong antibiotics through IV. But if the infection has spread to the bloodstream, you could go into septic shock. Even with the best care, 4 to 8% of people with Fournier’s gangrene die. For those who survive, recovery takes months. Some need multiple surgeries. Others live with permanent changes to their body.
What to Do Right Away
If you suspect Fournier’s gangrene, here’s what you must do:
- Stop taking your SGLT2 inhibitor immediately. Don’t wait for a doctor’s call. Don’t think it might be something else. Just stop.
- Go to the nearest emergency room. Tell them you’re on an SGLT2 inhibitor and you have symptoms of possible Fournier’s gangrene. Say the words out loud - it helps them act fast.
- Bring your medication bottle. The ER staff need to know exactly which drug you’re taking.
- Do not delay. If you’re in pain, swollen, or feverish - don’t call your GP. Don’t wait until morning. Go now.
Emergency teams are trained for this. They’ll check your blood, do a CT scan, and if they see gas in the tissue - a sign of bacterial invasion - they’ll take you to surgery within hours. Time is everything.
Who’s at Highest Risk?
Not everyone on SGLT2 inhibitors will get this. The risk is still very low - about 2 in 100,000 people per year. But some people are more vulnerable:
- Those with HbA1c over 9% - poor blood sugar control
- People with a history of genital yeast or bacterial infections
- Those with weakened immune systems - from steroids, chemotherapy, or HIV
- People with obesity or poor hygiene in the genital area
- Men over 50 - though women are at risk too
If you fit even one of these, talk to your doctor. You might still be a good candidate for the drug - but you need to be extra careful.

The Bigger Picture: Benefits vs. Risk
Let’s be clear: SGLT2 inhibitors save lives. They cut heart failure hospitalizations by up to 30%. They slow kidney disease in people with diabetes. For many, they’re the difference between needing dialysis and staying active into their 70s.
The FDA, the European Medicines Agency, and Australia’s TGA all still recommend these drugs - but with a warning. The benefits outweigh the risk for most people. But that doesn’t mean you can ignore the signs.
Doctors now train patients like this: "If you’re on this drug, treat any genital pain or swelling like you would a heart attack. Act fast. Don’t wait. Call 911. Go to the ER."
What Your Doctor Should Tell You
At your next appointment, ask: "Do I need to know about Fournier’s gangrene?" If they don’t bring it up, they’re not giving you full information. You deserve to know the risks.
Good doctors now use clear language: "This drug makes your urine sugary. That can lead to a rare but deadly infection. If you get pain, swelling, or fever in your groin, go to the ER right away. Don’t wait. Don’t call me. Go."
It’s not about scaring you. It’s about giving you power. You can keep the benefits of the drug - and avoid the worst outcome - if you know what to look for.
What Happens After You Recover?
If you survive Fournier’s gangrene, you’ll likely need to stop SGLT2 inhibitors for good. Your doctor will switch you to another class of diabetes medication - maybe a GLP-1 agonist like semaglutide, or insulin. You’ll also need to manage your blood sugar tighter than ever. And you’ll need to check your genital area daily for any changes.
Some patients need reconstructive surgery. Others deal with chronic pain or nerve damage. Recovery isn’t just physical - it’s emotional too. But knowing what to watch for next time? That’s how you protect yourself.
Can women get Fournier’s gangrene from SGLT2 inhibitors?
Yes. While most cases are reported in men, about one-third of cases in Europe and the U.S. occurred in women. The infection affects the genital and perineal area, which both men and women have. Any person on an SGLT2 inhibitor who notices swelling, pain, or discoloration in the genital area should seek emergency care - regardless of gender.
Is Fournier’s gangrene contagious?
No. Fournier’s gangrene is not contagious. It’s caused by bacteria already living in your body - like E. coli from your gut - that get into the tissue through a small break in the skin. You can’t catch it from someone else. But poor hygiene, diabetes, and the effects of SGLT2 inhibitors can make you more likely to develop it.
Should I stop my SGLT2 inhibitor if I have a yeast infection?
A yeast infection alone doesn’t mean you need to stop. These are common side effects of SGLT2 inhibitors. But if the infection doesn’t clear up with treatment, or if you start having pain, swelling, or fever, that’s a red flag. Contact your doctor immediately. Don’t wait for symptoms to get worse.
How long after starting an SGLT2 inhibitor can Fournier’s gangrene occur?
It can happen anytime - even after years of use. Most cases occur within the first year, but there are reports of it happening after 3, 5, or even 7 years on the drug. That’s why ongoing vigilance matters. Don’t assume you’re safe just because you’ve been on it a long time.
Are all SGLT2 inhibitors equally risky?
Yes. The risk appears to be a class effect. That means all drugs in this group - canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin - carry the same potential risk. It’s not one specific drug. It’s how the whole class works. Switching between them won’t reduce your risk.
Can I still take SGLT2 inhibitors if I’ve had a genital infection before?
You can - but you need to be extra careful. If you’ve had recurrent yeast or bacterial infections while on the drug, your doctor may recommend switching to a different class. Or they may advise you to monitor your genital area daily, keep it dry, and act immediately if anything feels off. The decision depends on your overall health and diabetes control.

9 Comments
I get that this is scary, but honestly? I’ve been on canagliflozin for 3 years and my genital area has never been more dry. Like, I’ve had yeast infections before - we all have - but this feels like fearmongering. The risk is 2 in 100k. You’re more likely to die from a vending machine falling on you.
Also, why is everyone acting like this is a new thing? It’s not. It’s just that now we have better reporting. Stop panicking. Just keep your area clean and check for rashes. That’s it./p>
Y’all need to hear this: if you’re on an SGLT2 inhibitor and you feel ANYTHING off down there - don’t wait. Don’t Google it. Don’t wait till morning. Go to the ER. Now.
I had a friend who waited because she thought it was a UTI. She lost part of her labia. And she’s lucky. She’s alive.
Yes the drug saved her kidneys. Yes it helped her lose 40 lbs. But this? This is non-negotiable. Your body will scream before it breaks. Listen. Please./p>
LOL so now we’re blaming the drug for bacteria that live in our own gut? 🤡
Let me guess - next they’ll say diabetes is what caused the infection? Nooooooo it’s the SGLT2 inhibitor’s fault because it makes urine sweet? So every diabetic who doesn’t take it is immune?
Also, 12 cases in 5 years? That’s less than a single plane crash. We’re acting like this is a pandemic. Meanwhile, 100k people die from heart failure every year and no one’s screaming to ban metformin.
Wake up. This is fear + profit. 💊🩸/p>
There’s something deeply human here. We’re told to trust science, but then we’re handed a warning that sounds like a horror movie.
On one hand, these drugs are miracles - they’re keeping people off dialysis, out of hospitals, alive longer. On the other, we’re being told to treat a rare symptom like a ticking bomb.
Maybe the real issue isn’t the drug. It’s that we’ve stopped teaching people how to listen to their own bodies. The warning signs are clear. The fear? That’s what we need to unlearn./p>
As a clinical pharmacist with over 15 years in endocrinology, I must emphasize: the risk-benefit profile of SGLT2 inhibitors remains overwhelmingly favorable for the vast majority of patients.
That said, patient education is paramount. The clinical presentation of Fournier’s gangrene is insidious and rapidly progressive. Delayed presentation correlates directly with increased mortality.
Therefore, we now include a mandatory patient safety sheet with all SGLT2 prescriptions, which includes explicit instructions to seek emergency care for any genital pain, swelling, or discoloration - regardless of perceived severity./p>
Let me break this down for you like you’re 12.
SGLT2 inhibitor = sugar in your pee.
Sugar in your pee = bacteria party.
Bacteria party + bad hygiene + high blood sugar = infection that eats your junk.
It’s not magic. It’s biology.
And yes, women get it too. Your vagina is not a forcefield.
Stop being a hero. If it hurts? Go. Now. No excuses. You’re not saving money by waiting. You’re saving a funeral./p>
I’ve been on empagliflozin for 4 years. No issues. But I do this: every shower, I check. Just a quick look. No big deal. Dry it well. Wear cotton. No tight jeans.
That’s it.
My doctor told me: 'If it stings, if it swells, if it smells - you don’t text. You don’t call. You drive.'
I did it once. Thought it was a pimple. Turned out to be a yeast infection. Took 2 weeks to clear.
So yeah. Be smart. Not scared. Just aware.
And if you’re scared? Talk to your doc. Not Reddit./p>
Oh wow. So now we’re telling diabetics to fear their own urine? Brilliant.
Let me guess - next they’ll ban insulin because it 'promotes bacterial growth in sweat glands.'
This is pure pharmacovigilance theater. The FDA gets paid to scare people. The pharma companies get paid to sell the next drug.
Meanwhile, people are dying from lack of access to care. But hey - at least we know not to pee in the shower. 🙃/p>
This is all part of the Great Diabetes Scam.
SGLT2 inhibitors were designed to make you dependent. The 'rare side effect' is just a way to push you into GLP-1 agonists - which cost 10x more.
Why do you think they added 'women can get it too'? To make the fear universal.
And why now? Because the patents are expiring.
Wake up. This isn’t medicine. It’s a business model./p>