
Chronic Hepatitis B Treatment Eligibility Calculator
Check Treatment Eligibility
Enter your child's lab results and medical history to determine if treatment is recommended according to current guidelines.
When a child is diagnosed with Chronic Hepatitis B is a long‑lasting infection of the liver caused by the hepatitis B virus (HBV). It can persist for years, sometimes decades, and may lead to liver damage if not managed properly. Parents often feel overwhelmed, wondering how the virus was caught, what the health outlook looks like, and which steps protect their kid’s future. This guide breaks down the science, the medical roadmap, and the everyday actions families can take.
What Exactly Is Chronic Hepatitis B?
HBV is a DNA virus that attacks liver cells. If the virus stays in the body for more than six months, doctors label it “chronic.” The condition differs from the short‑term “acute” infection, which usually clears on its own. Chronic infection means the virus continues to make copies, and the immune system lives with a low‑grade battle that can scar the liver over time.
How Do Children Usually Catch the Virus?
There are three main routes:
- Mother‑to‑child transmission - The most common way worldwide. The baby can pick up the virus while passing through the birth canal or during breastfeeding if the mother’s viral load is high.
- Household exposure - Sharing razors, toothbrushes, or any equipment that might have blood.
- Needle‑related contact - Rare in children, but possible in settings like tattooing or unsafe medical procedures.
Understanding the route helps doctors decide on preventive steps, especially the birth‑dose vaccine.
Signs, Symptoms, and When to Suspect Infection
Most kids feel fine. Chronic HBV often hides behind normal growth curves and school performance. When symptoms appear, they may include:
- Persistent tiredness
- Abdominal pain or swelling
- Jaundice - yellowing of skin or eyes
- Unexplained bruising
Because these signs overlap with many other conditions, a simple blood test is the reliable way to confirm infection.
Key Diagnostic Tests
Doctors rely on a panel of markers. The first clue is the presence of HBsAg (hepatitis B surface antigen) for more than six months. Additional tests include:
- HBeAg - indicates active viral replication.
- HBV DNA level - measures the amount of virus in the blood.
- ALT (alanine aminotransferase) - an enzyme that rises when liver cells are injured.
- Ultrasound - checks for any early signs of liver scarring.
All these results together help decide if treatment is needed now or can wait.

When Is Treatment Recommended?
Guidelines vary by country, but most experts agree on three main triggers for kids older than two years:
- HBV DNA>20,000IU/mL AND elevated ALT for at least three months.
- Evidence of liver inflammation on biopsy or imaging.
- Family history of liver cancer or cirrhosis, even if the child’s labs look okay.
If none of these criteria are met, doctors usually adopt a “watch‑and‑wait” approach, monitoring labs every 3‑6 months.
First‑Line Antiviral Options for Kids
Two oral medicines dominate the pediatric market. Both are taken once daily, have excellent safety records, and are approved for children as young as 2 years.
| Attribute | Tenofovir Disoproxil Fumarate (TDF) | Entecavir |
|---|---|---|
| Brand name | Viread | Baraclude |
| Age approved | 2years+ | 2years+ |
| Dosing | Weight‑based (5mg/kg) once daily | Weight‑based (0.015mg/kg) once daily |
| Resistance profile | Very low; resistant strains rare | Low; resistance can develop with long‑term use |
| Common side effects | Mild kidney function changes, occasional nausea | Headache, fatigue |
| Monitoring needed | Renal function every 6months | Liver enzymes every 3-6months |
Both drugs suppress viral replication, lower ALT, and improve long‑term liver health. The choice often hinges on the child’s kidney status, family preference, and the physician’s experience.
How to Start and Continue Treatment
- Baseline labs: HBV DNA, ALT, creatinine, and ultrasound.
- Pick the antiviral based on the table above.
- Prescribe the weight‑adjusted dose and give clear instructions on taking the pill with or without food.
- Schedule follow‑up labs at 1month, then every 3months for the first year.
- Adjust dose if the child gains weight or if labs suggest side effects.
Adherence is crucial. Missing doses can let the virus rebound, which makes future treatment harder.
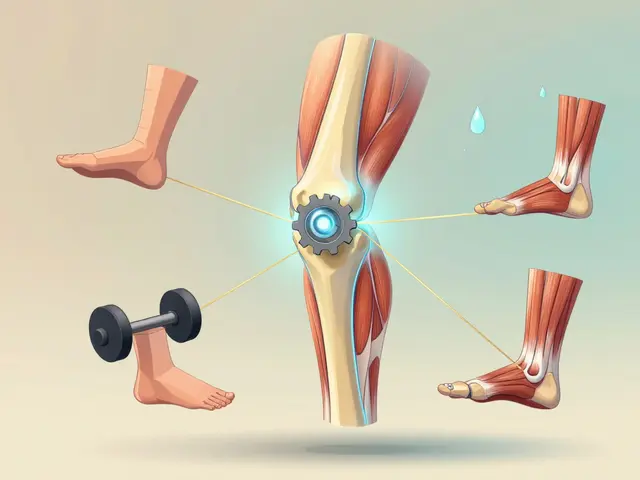
Long‑Term Monitoring and Lifestyle Tips
Even after viral suppression, doctors keep an eye on the liver for life. Typical follow‑up includes:
- ALT and HBV DNA every 6-12months.
- Ultrasound every 1-2years to spot early scarring.
- Screening for hepatitis D if the child lives in an endemic region.
Families can support liver health by:
- Encouraging a balanced diet rich in fruits, vegetables, and lean protein.
- Avoiding excess alcohol-most pediatric guidelines advise none.
- Staying active; regular exercise reduces liver inflammation.
- Keeping vaccinations up to date, especially the seasonal flu shot.

Vaccination: The Most Powerful Prevention
When a newborn receives the hepatitis B vaccine within 12hours of birth, the risk of mother‑to‑child transmission drops from up to 90% to under 5%. The routine schedule in Australia (and most high‑income nations) looks like:
- Birth dose (0months) - Recombivax‑HB (a recombinant hepatitis B surface antigen vaccine)
- Second dose at 1-2months.
- Third dose at 6months.
If a child is already infected, the vaccine does not cure the disease, but it can protect siblings and close contacts from catching HBV.
Emotional Support and Resources for Families
Learning that a child lives with a chronic virus can feel isolating. Parents should know they are not alone:
- Australian Hepatitis B Association offers counseling and peer‑support groups.
- Local pediatric liver clinics often host family education nights.
- Online forums such as HepBKids provide practical tips on school disclosures and travel safety.
Keeping open communication with the child-using age‑appropriate language-helps reduce anxiety and encourages adherence to medication.
Quick Takeaways for Busy Parents
- Chronic hepatitis B can be silent; regular blood tests are the only reliable way to track it.
- Treatment starts when viral load is high and liver enzymes stay elevated.
- Tenofovir and Entecavir are the go‑to antivirals for kids; both are safe and once‑daily.
- Birth‑dose vaccination cuts transmission risk dramatically.
- Long‑term monitoring, a healthy lifestyle, and emotional support keep your child thriving.
Frequently Asked Questions
Can a child outgrow chronic hepatitis B without treatment?
Some children maintain low viral loads and normal liver enzymes for years, but the virus usually stays in the body for life. Even when labs look good, regular monitoring is essential because flare‑ups can happen later.
Is it safe for my child to receive other vaccines while on antivirals?
Yes. Antiviral therapy does not interfere with routine immunizations. In fact, staying up‑to‑date on vaccines protects the liver from extra stress caused by infections.
What should I do if my child misses a dose of Tenofovir?
Take the missed dose as soon as you remember, unless it’s almost time for the next one. Never double‑dose; just continue with the regular schedule.
Can hepatitis B be transmitted through casual contact at school?
No. The virus spreads through blood or body fluids, not through shared toys, desks, or casual hugs. Good hygiene is always a plus, but there’s no need for isolation.
What are the long‑term risks if the virus stays untreated?
Over many years, chronic HBV can lead to liver fibrosis, cirrhosis, and hepatocellular carcinoma. Early treatment and consistent monitoring dramatically lower those risks.



9 Comments
Your summary overlooks the fact that the global mother‑to‑child transmission rate without immunoprophylaxis hovers around 90 %, not the 70 % you implied. Moreover, the risk drops below 5 % only when the birth‑dose vaccine is administered within 12 hours and the mother’s viral load is <200,000 IU/mL. The guidelines also stress that HBeAg‑positive mothers need antiviral prophylaxis in the third trimester, something the article barely touches. Lastly, the claim that tenofovir is always ‘kid‑friendly’ ignores its potential impact on bone mineral density in pre‑teens. A more nuanced take would save parents from false security.
/p>While the technical corrections are spot‑on, the article does a decent job of giving parents a clear action plan. It balances the heavy science with practical steps like scheduling regular ALT checks, which many newcomers find reassuring. The tone could be a touch warmer, but overall the guidance hits the mark for everyday families.
/p>Okay, I gotta say, the whole "no need to worry" vibe feels a bit dramatic, lol. Sure, the stats are scary, but most kids live normal lives with proper monitoring. If you’re obsessing over every lab number, you’ll miss the bigger picture – like the fact that HBV isn’t spread by sharing a pencil or hugging at school. Keep it real, but don’t let the fear monster take over ur day.
/p>Hey everyone, just wanted to add that staying positive really helps the kiddo cope. Even if there are typos in the guide, the heart of the message shines through – keep up with vaccines, meds, and those routine check‑ups. It’s okay to feel overwhelmed, but you’re doing great for your child’s future. Keep pushin’ forward!
/p>Kids can bounce back if you stay on schedule.
/p>From a clinical perspective, it is essential to emphasise that the decision to initiate antiviral therapy hinges upon a composite of virological and biochemical markers, rather than a single isolated value. The threshold of HBV DNA >20,000 IU/mL combined with persistently elevated ALT for three months constitutes a well‑validated trigger for treatment in paediatric patients. Additionally, the choice between tenofovir disoproxil fumarate and entecavir should consider renal function, as tenofovir may precipitate nephrotoxic effects in predisposed individuals. Regular renal monitoring, typically every six months, aligns with current best practice guidelines. Ultimately, a multidisciplinary approach involving hepatology, paediatrics, and pharmacy ensures optimal outcomes.
/p>When navigating chronic hepatitis B in children, the first step is to understand that the virus is remarkably resilient, but not invincible. Regular monitoring of HBV DNA levels provides a clear picture of viral activity and helps clinicians decide when to intervene. Equally important is tracking ALT, as sustained elevation often signals ongoing liver inflammation that warrants attention. The birth‑dose vaccine remains the most effective preventive measure, reducing transmission rates from nearly 90 % down to under 5 % when administered promptly. For mothers with high viral loads, third‑trimester antiviral prophylaxis, typically with tenofovir, adds an extra layer of protection for the newborn. Once a child is diagnosed, the decision to start therapy hinges on a combination of factors: viral load, ALT trends, liver imaging, and family history of hepatocellular carcinoma. Tenofovir and entecavir are the two frontline agents, each with a favourable safety profile, yet they are not interchangeable in every scenario. Tenofovir, while effective, requires periodic assessment of kidney function to preempt potential nephrotoxicity. Entecavir, on the other hand, may be preferred in children with pre‑existing renal concerns, but long‑term liver monitoring remains essential. Adherence cannot be overstated; missed doses can lead to viral rebound, resistance development, and a more complicated treatment course later on. Parents should establish a routine, perhaps tying medication intake to a daily activity like brushing teeth, to reinforce consistency. Lifestyle modifications, such as a balanced diet rich in antioxidants, regular physical activity, and avoidance of alcohol, support liver health alongside pharmacotherapy. Emotional well‑being is also critical – children who feel supported and informed are more likely to cooperate with treatment plans. Support groups, both in‑person and online, can provide valuable peer insight and reduce the sense of isolation that families often experience. Finally, lifelong surveillance, including periodic ultrasounds and alpha‑fetoprotein testing, helps catch any early signs of fibrosis or malignancy, ensuring that interventions can be timely and effective.
/p>I appreciate the thorough walkthrough; it really bridges the gap between medical jargon and everyday understanding. By emphasizing both the science and the practical steps, we give families a roadmap that feels both doable and hopeful.
/p>Exactly right – the key is blending accurate medical guidance with empathy. If anyone needs resources, the Australian Hepatitis B Association offers multilingual pamphlets and virtual counseling that can make the journey less daunting for both kids and parents.
/p>