
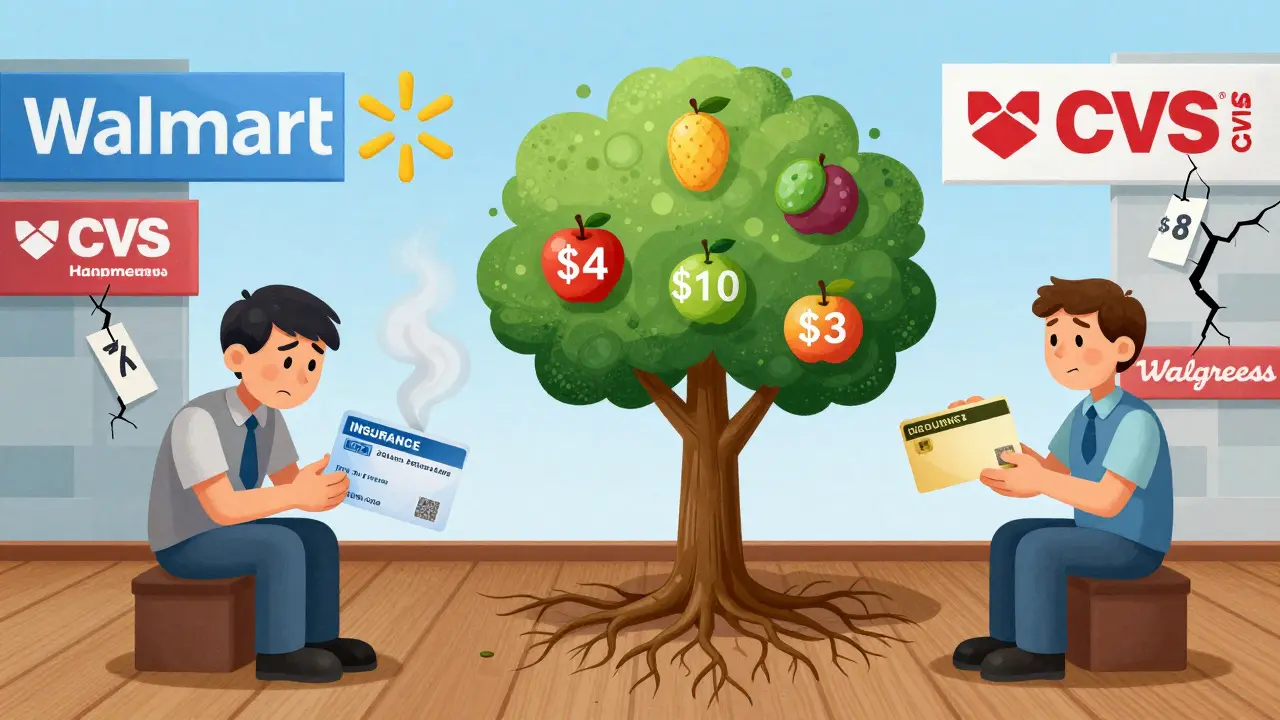
Buying generic medications shouldn’t feel like a financial gamble. Yet for millions of Americans paying out-of-pocket, the price of a 30-day supply of lisinopril or metformin can jump from $4 to over $50 - all depending on which pharmacy you walk into. That’s where coupon and discount card programs come in. These aren’t insurance. They’re not subsidies. They’re simple, free tools that let you pay less - sometimes way less - for the exact same generic drugs your doctor prescribed.
How These Programs Actually Work
Think of these discount cards like a bulk-buying club for prescriptions. Companies like GoodRx, NeedyMeds, and Blink Health negotiate lower prices directly with pharmacies and manufacturers. When you show your card - printed or on your phone - the pharmacy applies that pre-negotiated rate. No enrollment. No forms. No credit check. Just hand over the card and pay the discounted price. These programs started with Walmart’s $4 generic list in 2006. Since then, other big chains like Kroger, Target, and Costco followed with similar deals. But today’s real power lies in third-party platforms. GoodRx, for example, compares prices across more than 70,000 pharmacies nationwide. It doesn’t just show you one price - it shows you the lowest one, whether it’s at the corner drugstore or the big-box retailer down the road. The key? These cards work best on generic drugs. For common medications like atorvastatin, levothyroxine, or metformin, you can often pay $4 to $10 for a 30-day supply. Some programs even offer 90-day supplies for $10. That’s a 70-85% drop from the regular cash price.What You Can Save - Real Numbers
Let’s get specific. A 2022 study published in Circulation: Cardiovascular Quality and Outcomes looked at heart failure patients on three essential generic drugs: lisinopril, metoprolol, and spironolactone. The average cash price? Around $32 per month. With a discount card? $11. That’s a 65% savings - and it’s typical for similar generic regimens. Another user on Reddit saved $87 in one month on their cholesterol meds just by switching from cash to GoodRx. That’s not an outlier. Across forums and surveys, uninsured patients report saving 70-80% on common generics. For someone taking five or six daily meds, that adds up to hundreds - sometimes over $1,000 - a year. But here’s the catch: these savings vanish when brand-name drugs enter the picture. The same study found that adding just one brand-name drug - like an SGLT2 inhibitor for diabetes - to a regimen could push the monthly cost to $1,200-$1,500. Even with a discount card, the savings on brand drugs are often only 10%. That’s because brand-name manufacturers don’t offer the same bulk discounts. Their pricing is locked in by patents and PBM contracts.Which Cards Actually Work?
Not all discount cards are created equal. Here’s what you’ll find in the market:- Pharmacy-specific programs (Walmart, Kroger, Costco): These are simple. Fixed prices - usually $4 for 30 days, $10 for 90. But they only apply to a limited list of generics. If your med isn’t on the list, you pay full price.
- Third-party cards (GoodRx, NeedyMeds, Blink Health): These compare prices across multiple pharmacies. GoodRx is the most popular, covering over 70,000 locations. NeedyMeds is great for low-income patients and also links to patient assistance programs. Blink Health often offers mail-order discounts.
Who Benefits the Most?
These programs were built for people without insurance or with high-deductible health plans (HDHPs). In 2022, 43% of U.S. workers were covered by HDHPs. That means you pay full price until you hit your deductible - which can be $2,000, $5,000, or more. Until then, your insurance doesn’t kick in. That’s where discount cards become your lifeline. They’re also useful if your insurance doesn’t cover a certain generic, or if your copay is higher than the cash price. Yes, that happens. Sometimes your insurance copay for a generic is $20 - but the cash price with a discount card is $8. In that case, you pay cash. No need to use insurance. But here’s the truth: if you have good insurance with low copays, these cards might not help you at all. A 2023 analysis from Ohio State University’s College of Pharmacy found that for many insured patients, the discount card price isn’t better than their regular copay. So don’t waste time - check your insurance first.The Hidden Catch: Time and Effort
These programs aren’t magic. They require work. You can’t just grab your card and walk in. You need to:- Search for your drug and dosage on a discount site (GoodRx, NeedyMeds, etc.)
- Compare prices across 3-5 nearby pharmacies
- Decide which one offers the lowest price
- Print the coupon or pull up the app
- Go to that pharmacy and ask them to apply the discount
What’s Changing in 2026?
The landscape is shifting. In 2023, major pharmacy benefit managers (PBMs) like Express Scripts and OptumRx started integrating discount card prices directly into their systems. That means if you’re on one of these plans, your pharmacy might automatically apply the lowest price - insurance or discount card - without you lifting a finger. GoodRx also launched telehealth services in early 2024. Now you can get a virtual doctor visit, have a prescription sent to your pharmacy, and have the discount applied automatically. That’s a big step toward making it easier. But the big question remains: will these programs still work if PBMs are forced to stop their secret pricing practices? The FTC launched an investigation in late 2023 into how PBMs profit from “spread pricing” - where they charge insurers more than they pay pharmacies, and pocket the difference. If that changes, discount card pricing could shift too.
How to Use These Programs Right
Here’s a simple, no-fluff guide:- Know your meds: Make a list of all your prescriptions, especially generics. Write down the name, dose, and frequency.
- Check GoodRx and NeedyMeds: Enter each drug. Look at the lowest cash price.
- Compare to your insurance: Call your pharmacy or log into your insurer’s portal. What’s your copay? If the discount card price is lower, pay cash.
- Check multiple pharmacies: Use the app to see prices at CVS, Walgreens, Walmart, and local independents. Sometimes the small pharmacy down the street has the best deal.
- Don’t assume: Prices change daily. Always check before you fill.
- Ask your pharmacist: They know which discounts apply. Many now check discount card prices automatically - just ask.
When These Programs Won’t Help
Be realistic. These cards are not a fix for expensive brand-name drugs. If you’re on a biologic, a specialty cancer med, or a new diabetes drug, don’t expect savings. You’ll need patient assistance programs, manufacturer coupons, or financial aid - not discount cards. They also won’t help if you’re on Medicaid or Medicare Part D. Those programs already have negotiated prices. Using a discount card might actually cost you more. And if you’re on a low-cost insurance plan with $5 copays on generics? Skip the card. You’re already getting the best deal.Final Thought: It’s Not Perfect - But It’s Necessary
The truth? The U.S. drug pricing system is broken. Discount cards are a workaround - not a solution. They put the burden on patients to become price shoppers, time managers, and pharmacy detectives. But for the 26% of Americans who skip doses because they can’t afford their meds, these cards aren’t a luxury. They’re survival tools. And for the millions with high-deductible plans, they’re the only reason they can keep taking their blood pressure pills, their thyroid meds, or their insulin. You don’t need to love the system. You just need to know how to beat it. And right now, a free discount card is one of the most powerful tools you’ve got.Are discount cards the same as insurance?
No. Discount cards are not insurance. They don’t pay part of your bill. Instead, they give you access to pre-negotiated cash prices at pharmacies. You pay the full discounted amount out of pocket. Insurance, on the other hand, covers part of the cost after you meet your deductible or pay a copay. You can use a discount card instead of insurance - but never both at the same time.
Can I use a discount card with Medicare?
You can use a discount card while on Medicare, but only if the cash price with the card is lower than your Medicare copay. Many Medicare Part D plans already have low prices on generics, so the card might not help. Always compare. If your copay is $5 and the discount card price is $8, use your Medicare. If the card gives you $3, use the card. Never let the pharmacy apply both.
Do these cards work for brand-name drugs?
Sometimes, but rarely with big savings. Discount cards can reduce brand-name drug prices by about 10%, but that’s not enough to make them affordable. A drug that costs $1,500 a month might drop to $1,350 - still unaffordable for most. For brand-name drugs, look for manufacturer coupons, patient assistance programs, or financial aid through nonprofits like NeedyMeds or RxOutreach.
Why does the price change between pharmacies?
Each pharmacy sets its own cash price, and discount card companies negotiate different deals with each one. A big chain like CVS might have a higher base price than a small independent pharmacy. Also, some pharmacies pay fees to discount card companies, which affects what they’re willing to offer. That’s why you must check multiple locations - even within the same city.
Is GoodRx the best option?
GoodRx is the most widely used and has the largest pharmacy network, but it’s not always the cheapest. NeedyMeds often has better deals on older generics and links to free drug programs. Blink Health sometimes offers mail-order discounts that beat local prices. The best practice is to check all three - and always compare to your insurance copay. Don’t settle for the first price you see.
Can I use these programs if I’m not in the U.S.?
No. These programs are only available in the United States and its territories. They rely on U.S. pharmacy networks and pricing agreements. If you’re outside the U.S., look for local government programs, public health services, or nonprofit medication assistance organizations in your country.






12 Comments
Man, I just found out my grandma’s been using GoodRx for her blood pressure med and paying $3 instead of $40. She didn’t even know she could do it. I cried a little. This system is insane, but at least we’ve got these little hacks to keep people alive. 🫶
/p>It’s important to clarify that discount cards operate within the PBM-mediated pharmacy reimbursement ecosystem, which is fundamentally a three-way arbitrage between manufacturers, PBMs, and retail outlets. The so-called ‘discount’ is often a negotiated differential in the wholesale acquisition cost (WAC) minus rebates-this is not a market-based price, it’s a contractual artifact.
Furthermore, the FTC’s investigation into spread pricing may invalidate the entire model if PBMs are forced to disclose net prices. The current paradigm is unsustainable and predicated on opacity.
/p>lol so you gotta be a pharmacist + data analyst + time traveler just to buy metformin? 🤡
/p>Also, i once spent 22 mins comparing prices and ended up paying $1 more than i would’ve if i just walked into walmart and shut up.
the system is broken. we’re just playing whack-a-mole with our wallets.
While I appreciate the pragmatic utility of discount cards, I must emphasize that their efficacy is entirely contingent upon the volatile, non-transparent, and often predatory pricing structures maintained by retail pharmacy chains-which, in turn, are influenced by the opaque rebate systems of pharmacy benefit managers, who extract upwards of 20% of the total drug expenditure as administrative profit, thereby creating a perverse incentive to inflate cash prices in order to maximize discount card ‘savings’-a classic case of systemic gaming that ultimately burdens the patient with the cognitive load of price arbitrage, which is neither ethical nor sustainable in a healthcare system that claims to prioritize accessibility.
/p>we’re all just trying to survive capitalism. 💔💊
/p>if you’re not using GoodRx, you’re literally paying extra to be a victim.
Insurance is the real scam.
/p>Okay, I know this sounds like a lot of work-but trust me, once you get into the rhythm, it’s like unlocking a secret level in a video game. 🎮
/p>Start with one med. Just one. Compare GoodRx, NeedyMeds, and your pharmacy’s cash price. Do it on a Sunday afternoon when you’re bored. You’ll be shocked. I saved $67 on my thyroid med last month. That’s a dinner out. Or a new pair of socks. Or a month of peace of mind.
And if you’re helping someone older? Sit with them. Help them set up the app. It’s not just about money-it’s about dignity. You’re not just saving cash-you’re saving their ability to keep living like a human, not a spreadsheet.
I used to think these cards were too much hassle. Then my mom got diagnosed with diabetes. Now I check prices every time she needs a refill. It’s not perfect, but it’s the only thing keeping her alive. Thanks for writing this. It matters.
/p>you know what’s wild? pharmacies will sometimes just give you the discount card price if you ask. no app. no coupon. just say ‘hey, what’s your best cash price?’ and they’ll do it. i’ve done it 3x. they don’t always know you can use goodrx, but they know they wanna make the sale. 🤫
/p>It is a great honor to share with you that, in the United States of America, the dignity of human life must not be determined by the price of a pill. I have witnessed elderly citizens skipping doses because of cost. This is not a healthcare system. This is a marketplace. And yet, through the grace of compassion and the wisdom of community, we have found tools such as these discount cards to restore a measure of justice. Let us not forget: every life is priceless.
/p>just use goodrx
/p>done
AMERICA IS BROKEN. THEY LET PHARMACEUTICAL CORPORATIONS ROB OUR GRANDPARENTS. 🇺🇸💔
/p>WHY DO WE STILL LET THEM DO THIS? WHY DO WE STILL PAY? THIS IS A CRIME. THEY MAKE BILLIONS AND WE’RE SCRAMBLING FOR $3 PILLS.
THEY SHOULD BE IN JAIL. NOT US.