
Psoriasis isn’t just a rash. It’s a lifelong condition that changes how your body works - inside and out. If you’ve been told you have psoriasis, you’re not alone. Around 2-3% of people worldwide live with it, and in places like Scandinavia, that number jumps to 2.5%. In Australia, it affects roughly 1 in 50 people. The red, scaly patches on your skin are just the visible part. Underneath, your immune system is stuck in overdrive, making skin cells race to the surface in just 3-4 days instead of the normal 28-30. That’s why plaques build up so fast.
What Psoriasis Actually Looks Like
Most people with psoriasis have plaque psoriasis - about 80-90% of cases. These are thick, red patches covered in silvery scales, usually on elbows, knees, scalp, and lower back. But it’s not always that simple. Some get inverse psoriasis - smooth, shiny red patches in skin folds like the groin, under breasts, or between buttocks. These hurt more from sweat and friction than from scaling. Others develop guttate psoriasis after a strep throat - tiny drop-like spots all over the body. Pustular psoriasis shows up as white, pus-filled bumps, often on hands or feet. And then there’s erythrodermic psoriasis, rare but dangerous: your whole skin turns red, peels off, and can throw your body temperature and fluids out of balance. That’s a hospital emergency.It’s Not Just Skin Deep
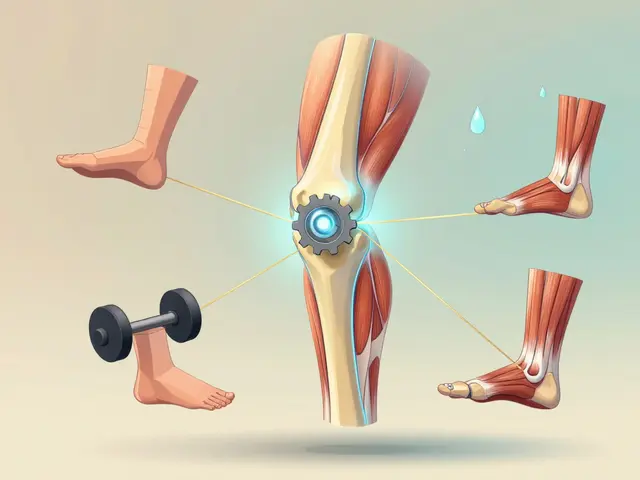
Many think psoriasis is just a skin problem. It’s not. It’s a systemic disease. Up to 30% of people with psoriasis develop psoriatic arthritis - joint pain, stiffness, swelling, especially in fingers, toes, and lower back. Nail changes like pitting or lifting are a big red flag. But the risks go further. People with psoriasis have a 58% higher risk of heart attack before age 50. One in two have metabolic syndrome - high blood pressure, high blood sugar, excess belly fat, and bad cholesterol. Depression and anxiety are three times more common than in the general population. Your skin is screaming about what’s happening inside. That’s why every check-up should include blood pressure, cholesterol, and mood screening. Ignoring these isn’t an option.Topical Treatments: Where It Starts
For mild cases, creams and ointments are the first step. Doctors often start with a combo of calcipotriol (a vitamin D analog) and betamethasone (a steroid). It works fast - plaques flatten in weeks. But steroids can’t be used forever. On thin skin like the face, groin, or eyelids, they cause thinning, red veins, and stretch marks. That’s why scalp psoriasis gets a foam, the face gets vitamin D alone, and the genitals get low-potency steroids. The key? Consistency. People who apply treatments once a day instead of twice are 40% more likely to stick with them. Use moisturizers daily - petrolatum-based ones work best. Keep showers short and lukewarm. Harsh soaps dry out skin and make plaques worse.When Topicals Aren’t Enough
If your plaques cover more than 5% of your body, or if they’re on your face, hands, or scalp and affecting your life, you need more than creams. Phototherapy - narrowband UVB light - is next. You go to the clinic 2-3 times a week for 8-12 weeks. It clears 75% of plaques for many. Home units cost $2,500-$5,000 upfront, plus monthly maintenance. Some people avoid this because of time or cost. Others find it works better than pills. Then come the oral systemic drugs: methotrexate (weekly pills), acitretin (a vitamin A derivative), or cyclosporine (for severe flare-ups). Methotrexate can cause nausea and liver stress. Cyclosporine affects kidneys. These aren’t for everyone, but they’re powerful tools when used right.Biologics: The Game Changers
Biologics changed everything. These are injectable or IV drugs that block specific parts of the immune system driving psoriasis. You don’t take them daily - often once a month or every few weeks. They’re not cures, but they can get you to near-clear skin. Drugs like secukinumab, guselkumab, and adalimumab target IL-17, IL-23, or TNF-alpha. In trials, 58-75% of patients hit PASI90 - meaning 90% of their plaques disappeared. That’s life-changing. On Healthgrades, users give biologics a 4.3/5 rating for effectiveness. But cost is brutal. Without good insurance, monthly bills can hit $1,200-$5,500. Even with coverage, co-pays often hit $350/month. That’s why 41% of patients delay or skip doses. And if you start a biologic, you need TB and hepatitis tests first. It’s not just about the injection - it’s about safety checks.
Why People Stop Treatment
The biggest problem? Sticking with it. Half of people on systemic treatments quit within a year. Why? Side effects. Nausea from methotrexate. Worries about kidney damage from cyclosporine. The hassle of injections. The cost. And let’s be honest - some feel better after a few months and think they’re cured. They stop. Then the plaques come back, worse than before. On Reddit’s psoriasis community, 67% of users say topical creams are messy and hard to use consistently. 58% worry about steroids, even when they work. The solution? Simplify. Use once-daily combos. Use apps like MyPsoriasisTeam to track flare-ups and meds. Join support groups. You’re not failing - the system is hard. But you’re not alone.What’s Coming Next
The future is faster, easier, and more personal. Deucravacitinib, a pill approved in 2022, works by blocking a different immune pathway (TYK2). In trials, it gave PASI90 to 58% of users - without injections. Oral RORγt inhibitors are in Phase 2 and look just as strong. The goal now isn’t just symptom control - it’s near-complete clearance. New guidelines say your target should be PASI ≤3 and DLQI ≤4 - meaning almost no plaques and minimal impact on daily life. But here’s the catch: only 25-30% of moderate-to-severe patients get the right treatment. Rural areas have fewer dermatologists. Insurance fights are common. And biologics still cost 80% of research dollars. The system isn’t keeping up. But the science is. The future is matching your genes to your treatment - not guessing.Living With Psoriasis Today
You can’t cure it. But you can control it. Daily moisturizing. Avoiding triggers like stress, alcohol, or smoking. Tracking flares in a journal. Getting your heart and joints checked yearly. Talking to your doctor about what’s realistic. Biologics aren’t magic - they’re tools. Topicals aren’t weak - they’re the foundation. The best plan isn’t the most expensive one. It’s the one you can stick with. If your skin is clearing and your joints feel okay, you’re doing better than most. And if you’re struggling with cost or side effects? Ask. There are patient assistance programs, biosimilars coming, and new options every year. Psoriasis is chronic. But it doesn’t have to define you.Can psoriasis be cured?
No, psoriasis cannot be cured with current treatments. It’s a lifelong autoimmune condition. But it can be managed effectively. Many people achieve near-complete skin clearance with biologics or phototherapy, and symptoms can stay under control for years with consistent treatment and lifestyle adjustments.
Are biologics safe for long-term use?
Biologics are generally safe for long-term use when monitored by a dermatologist. They suppress specific parts of the immune system, so risks include increased susceptibility to infections like tuberculosis or hepatitis. Before starting, patients are screened for these. Regular blood tests and check-ups help manage risks. Most people tolerate them well for years, especially when benefits outweigh potential side effects.
Why do psoriasis treatments stop working over time?
Some treatments lose effectiveness because the immune system adapts. This is more common with older systemics like methotrexate. With biologics, it’s less frequent, but still possible - called "secondary failure." Switching to a different class of biologic (e.g., from a TNF blocker to an IL-17 inhibitor) often restores results. Your doctor can adjust your plan based on your response and disease activity.
Can diet or supplements cure psoriasis?
No diet or supplement can cure psoriasis. However, some people notice fewer flares when they reduce alcohol, lose weight, or follow an anti-inflammatory diet rich in omega-3s. Vitamin D supplements may help if you’re deficient, but they won’t replace topical or systemic treatments. Don’t rely on unproven remedies - they can delay effective care.
How do I know if my psoriasis is getting worse?
Signs include spreading plaques, new joint pain or stiffness, increased itching or burning, nails lifting or pitting, or feeling more tired or depressed. If your current treatment isn’t keeping your skin clear or your quality of life is dropping, it’s time to talk to your doctor. Tools like the PASI and DLQI scores help track progress objectively.
Is psoriasis contagious?
No, psoriasis is not contagious. You cannot catch it from touching someone’s skin, sharing towels, or being near them. It’s caused by genetics and immune system dysfunction, not bacteria or viruses. Misunderstanding this leads to stigma - which is why education matters.
What’s the best way to apply topical treatments?
Apply creams or ointments to clean, dry skin after a short lukewarm shower. Use a thin layer - more isn’t better. Rub it in gently. Don’t scrub. For scalp plaques, use foam or solution formulations. For sensitive areas like the face or genitals, use only mild products as directed. Consistency matters more than strength - applying once daily is better than skipping days.
Can psoriasis affect my mental health?
Yes, significantly. Studies show 17-37% of people with psoriasis experience depression or anxiety, compared to 6-7% in the general population. The visible nature of the condition, social stigma, and chronic discomfort contribute. Mental health screening should be part of every psoriasis check-up. Support groups, counseling, and apps like MyPsoriasisTeam can help reduce isolation and improve coping.


9 Comments
Been dealing with this for 12 years. Topicals are a pain but they work if you don’t skip. I use the calcipotriol/betamethasone combo once a day on my elbows and knees. No more double application nonsense. Moisturize right after shower, even if you’re tired. It’s not glamorous, but it keeps me out of the doctor’s office.
/p>Also, don’t listen to people who say "just eat better". I eat clean, still got plaques. It’s autoimmune, not a diet problem.
One must question the pharmaceutical hegemony that promotes biologics as panaceas. The cost structure is predatory, and the long-term immunosuppressive effects remain inadequately studied. One wonders if the true agenda lies not in healing, but in sustaining perpetual dependency on high-margin biologics.
/p>bro i tried that steroid cream and my face started peeling like a snake. now i just let it be. if it don’t hurt, why fight it? also i smoke and drink and still got the plaques so idk man.
/p>psoriasis is not a rash its a whole vibe
/p>you got the scalp flakes the joint pain the shame of showing your arms at the pool
but also the weird pride when you finally find something that works
biologics saved my life no cap
even if i have to cry over the insurance form every month
and yes i still use petroleum jelly like its holy water
psoriasis fam unite
It is imperative to recognize that the pathophysiology of psoriasis transcends mere cutaneous manifestations. The systemic inflammatory burden necessitates a holistic, multidisciplinary approach. One must not underestimate the role of metabolic comorbidities, nor the psychological toll, which often remains unaddressed in primary care settings.
/p>My mom had it bad. I used to help her put on the cream when I was 10. Now I have it too. Not as bad, thank god. But I get it. The shame, the itch, the weird looks. I don’t post pics of my legs on Instagram. But I do moisturize every night. And I tell my doctor everything - even the depression stuff. It’s not weak to ask for help.
/p>So you’re telling me I spent 8 years avoiding showers because I thought water made it worse… and the real villain was… hot water and Dove soap? 🤦♂️
/p>Also, biologics cost more than my rent. But hey, at least my skin doesn’t look like a crumpled map of Mars anymore. Small wins.
Let’s be real - the entire medical-industrial complex is built on chronic conditions. Psoriasis? Perfect. No cure, lifelong treatment, expensive drugs, insurance hoops, and patients who feel guilty for not being ‘compliant.’
/p>Meanwhile, the real breakthroughs - like the TYK2 inhibitor - get buried under patent wars and formulary restrictions. And don’t get me started on how dermatologists barely spend 7 minutes per visit. You’re not failing. The system is designed to keep you struggling. The fact that you’re even reading this means you’re already ahead of 90% of patients who just give up.
And yes, I know someone who took methotrexate and got liver fibrosis. And yes, they were told it was ‘rare.’ Rare doesn’t mean ‘won’t happen to you.’
Biologics aren’t magic. They’re expensive bandaids on a broken immune system. But until we fix the root cause - which nobody’s even trying to - we’re just rearranging deck chairs on the Titanic. And the Titanic? It’s called capitalism.
The epigenetic modulation of immune dysregulation in psoriasis presents a fascinating intersection between environmental triggers and genetic predisposition. The chronic inflammatory cascade, mediated primarily through the IL-23/Th17 axis, not only drives keratinocyte hyperproliferation but also contributes to systemic endothelial dysfunction - hence the heightened cardiovascular risk profile. When we consider the DLQI as a proxy for quality of life, it becomes ethically imperative to prioritize patient-centered outcomes over cost-efficiency metrics.
/p>Furthermore, the psychological burden, often underdiagnosed due to diagnostic overshadowing, necessitates integrated behavioral health protocols within dermatological care pathways. The emergence of oral small-molecule inhibitors represents a paradigm shift - not merely in delivery, but in accessibility - potentially reducing the treatment gap in underserved populations. Yet, the persistent disparity in access to biologics across socioeconomic strata remains a moral indictment of our healthcare infrastructure. We must move beyond symptom suppression toward true disease modification - and that requires policy reform as much as pharmacologic innovation.