
Diabetic retinopathy isn’t just a complication of diabetes-it’s the leading cause of preventable vision loss in adults under 65. If you have diabetes, your eyes are at risk. But here’s the good news: diabetic retinopathy can be caught early, and in most cases, vision loss can be avoided entirely. The key is knowing when to get screened and what treatments actually work.
When Should You Get Screened?
Screening for diabetic retinopathy isn’t one-size-fits-all. For years, the default was an annual eye exam. But research has changed that. Today, screening intervals are based on your individual risk-not just how long you’ve had diabetes.If you have type 1 diabetes, your first eye exam should happen 3 to 5 years after diagnosis. For type 2 diabetes, it’s recommended right after diagnosis because many people already have early signs of retinopathy by the time they’re diagnosed.
Here’s how screening frequency breaks down based on what the eye doctor finds:
- No retinopathy or mild nonproliferative DR: You can safely wait 1 to 2 years before your next exam. Some low-risk patients with stable blood sugar and no other complications may even stretch that to 3 years.
- Moderate nonproliferative DR: You need to be seen every 3 to 6 months. This is the warning stage-your blood vessels are starting to leak, and if left unchecked, it can escalate quickly.
- Severe nonproliferative DR: You need to see a specialist within 3 months. At this point, your retina is starving for oxygen. New, fragile blood vessels are forming, and they can bleed.
- Proliferative DR: This is an emergency. You need to be evaluated within a month. These new blood vessels are unstable. One minor bleed can cloud your vision or cause a retinal detachment.
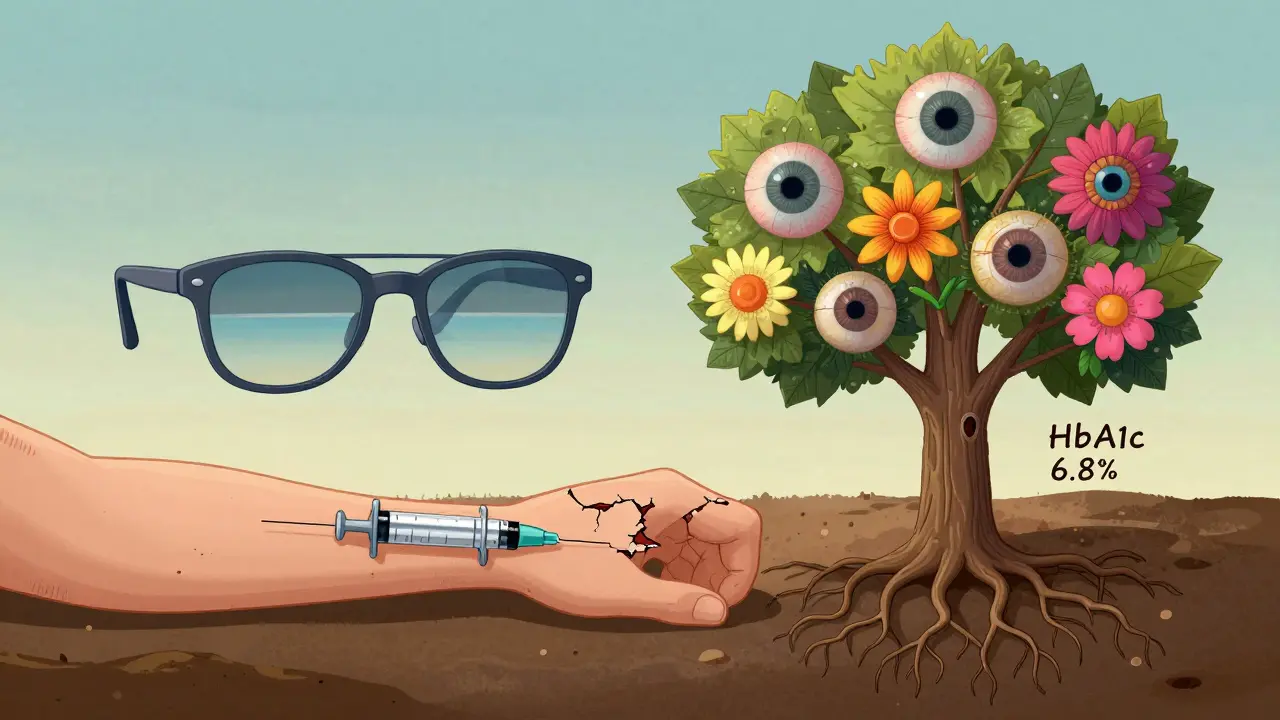
There’s also a tool called RetinaRisk that helps doctors calculate your personal risk. It looks at your HbA1c, how long you’ve had diabetes, your blood pressure, and kidney function. People with low scores might only need screening every 3 to 5 years. High-risk patients-those with HbA1c above 9%, high blood pressure, or kidney disease-need more frequent checks.
Studies show that switching from annual screenings to risk-based schedules can cut the number of eye visits by nearly 60% without increasing the chance of vision loss. That means less time off work, lower costs, and less anxiety for patients who’ve had clean results for years.
What Happens During a Screening?
A diabetic eye screening isn’t just a quick glance. It’s a detailed digital photo of the back of your eye. The standard is two images per eye, taken with a special camera after dilating your pupils. This gives doctors a clear view of the retina, blood vessels, and optic nerve.Some clinics now use AI-powered tools to analyze the images. Google’s DeepMind algorithm, for example, can spot signs of retinopathy with 94.5% accuracy-comparable to expert ophthalmologists. In rural areas where eye specialists are scarce, telemedicine screening with smartphone adapters like the D-Eye device is making a big difference. These tools let primary care providers take retinal photos during a regular checkup, then send them to a specialist for review.
Don’t be surprised if your vision is blurry for a few hours after the exam. That’s normal. The drops dilate your pupils so the camera can see everything. Bring sunglasses and plan for someone to drive you home.
Treatment Options for Diabetic Retinopathy
If your screening finds early signs of damage, the first line of defense isn’t surgery-it’s better control of your diabetes.The DCCT and EDIC studies proved that keeping your HbA1c below 7% cuts the risk of retinopathy progression by more than half. Lowering blood pressure and managing cholesterol also helps. In fact, one study found that tight control of both blood sugar and blood pressure reduced the risk of vision loss by 76%.
When damage is more advanced, treatments kick in:
- Anti-VEGF injections: These are the most common treatment for diabetic macular edema (DME) and advanced retinopathy. Drugs like ranibizumab and aflibercept block a protein that causes leaking blood vessels. You get injections directly into the eye, usually every 4 to 8 weeks at first, then less often as your condition improves. Most patients see improved or stabilized vision after a few months.
- Laser therapy: Focal laser treatment seals off leaking vessels in the macula. Panretinal photocoagulation (PRP) burns small areas of the retina to reduce oxygen demand and stop new blood vessels from forming. It’s not glamorous, but it’s been saving vision since the 1980s. It can cause some peripheral vision loss or night vision issues, but it prevents total blindness.
- Vitrectomy: If you’ve had a major bleed into the vitreous gel inside your eye, or if scar tissue is pulling on your retina, you may need surgery. A vitrectomy removes the cloudy gel and scar tissue, letting light reach the retina again. It’s done under local anesthesia and usually requires a few weeks of recovery.
There’s no magic cure. But with early detection and the right treatment, up to 98% of severe vision loss from diabetic retinopathy can be prevented.
Who’s at Highest Risk?
Not everyone with diabetes develops retinopathy. But some people are far more likely to. These are the red flags:- HbA1c consistently above 8%
- Diabetes duration longer than 15 years
- Systolic blood pressure above 140 mmHg
- Chronic kidney disease (eGFR below 60)
- Pregnancy (women with diabetes need monthly screenings during pregnancy)
- High cholesterol or smoking
Even if your HbA1c is under control, if you’ve had fluctuating levels over time-like jumping from 6.5% to 9.5% and back-that variability itself increases your risk. Stability matters as much as the number.
Low-income communities face higher rates of vision loss, not because they’re more likely to get diabetes, but because they’re less likely to get screened. In the U.S., only about 60% of people with diabetes get their recommended eye exams. That gap is where preventable blindness happens.
What’s New in 2026?
The biggest shift in 2026 is the move from fixed schedules to personalized plans. The American Diabetes Association’s 2024 guidelines now say: “Screening every 1-2 years may be considered if there’s no evidence of retinopathy and glycemic control is good.”AI screening is becoming standard in larger clinics. Insurance companies are starting to cover AI-based screenings as part of routine care. And new smartphone-based devices are making it possible for patients in remote areas to get high-quality images without traveling to a specialist.
There’s also growing interest in oral medications that might slow retinopathy progression. Early trials of drugs targeting inflammation and oxidative stress show promise, but they’re still years away from being widely available.
What Patients Are Saying
On diabetes forums, people are split. One user, Type1Warrior87, said: “After three clean screenings, my doctor switched me to every two years. I feel safer, not less cared for.”Another, RetinaScared2023, posted: “They pushed for biennial screening even though my HbA1c was 8.5%. I ended up with macular edema. I wish I’d pushed back.”
The message? Don’t let convenience override caution. If your numbers are high, don’t accept a longer interval just because it’s easier. Ask your doctor: “Based on my HbA1c, blood pressure, and kidney function, is my risk low enough for a longer gap?”
How to Stay Ahead
The best way to protect your vision isn’t waiting for your next screening-it’s managing your diabetes every day.- Check your blood sugar regularly. Don’t just rely on HbA1c.
- Keep your blood pressure under 130/80.
- Don’t smoke. Ever.
- Get your kidneys checked yearly.
- Ask your eye doctor for a copy of your retinal images. Track changes over time.
- If you’re pregnant, schedule monthly eye exams.
Diabetic retinopathy doesn’t cause pain. That’s why it’s so dangerous. By the time you notice blurry vision, it’s often too late. But if you’re proactive-screening on time, controlling your numbers, and speaking up when something feels off-you can keep your vision sharp for decades.
How often should I get screened for diabetic retinopathy if I have type 2 diabetes and no eye damage?
If you have type 2 diabetes and no signs of retinopathy, and your blood sugar and blood pressure are well controlled, you can safely wait 1 to 2 years between screenings. Some patients with very low risk-stable HbA1c under 7%, no kidney issues, and no hypertension-may extend that to every 3 years. But if your HbA1c is above 8% or you have high blood pressure, stick to annual exams.
Can diabetic retinopathy be reversed?
Early damage from diabetic retinopathy can be stabilized and sometimes improved with treatment, but the existing changes to blood vessels usually can’t be fully reversed. Anti-VEGF injections and laser therapy can stop leakage, reduce swelling, and prevent new abnormal vessels from forming. In some cases, vision improves after treatment, especially if macular edema is caught early. But once scar tissue forms or the retina detaches, permanent damage may occur.
Is laser treatment painful?
Laser treatment is usually done with local anesthesia, so you won’t feel pain during the procedure. You may feel pressure or see bright flashes of light. Afterward, your eye might feel sore or sensitive to light for a day or two. Some people notice a slight loss of peripheral or night vision, but that’s a trade-off to prevent total vision loss. Most patients tolerate it well and consider it a small price to pay for keeping their central vision.
Do I still need eye exams if I’m on insulin?
Yes. Being on insulin doesn’t protect you from retinopathy-it means your diabetes is more advanced and you’re at higher risk. In fact, people with type 1 diabetes on insulin need more frequent screenings than those with type 2. Your screening schedule should be based on your eye health and risk factors, not your medication. Insulin helps control blood sugar, but it doesn’t undo damage already done to the retina.
Can AI replace an eye doctor for diabetic retinopathy screening?
AI can analyze retinal images with high accuracy and is excellent at identifying referable disease-meaning cases that need a doctor’s attention. But it can’t replace a human eye doctor. AI doesn’t assess overall eye health, check for glaucoma or cataracts, or evaluate symptoms like sudden floaters or vision changes. It’s a tool to help screen more people faster, especially in underserved areas. If AI flags an issue, you still need to see an ophthalmologist for diagnosis and treatment.
What should I do if I can’t afford regular eye exams?
Many states and nonprofits offer free or low-cost diabetic eye screenings. Look for programs through your local health department, community clinics, or organizations like the American Diabetes Association. Some telemedicine platforms provide screenings for under $50. Medicare and most private insurers cover diabetic eye exams at least once a year. If you’re denied coverage, ask for a letter of medical necessity from your doctor. Preventing blindness is cheaper than treating it.






11 Comments
Bro this article is spot on but why are we still talking about annual screens like it's 2010? My doc switched me to every 2 years after my HbA1c dropped to 6.8 and my BP's been under 125/80 for a year. No drama no panic just facts. AI read my retinal pics better than the resident did last time.
/p>Life’s weird right? We’ll drive 40 mins for a latte but skip an eye exam because ‘it’s not urgent’ 😅 Diabetic retinopathy doesn’t scream it’s coming-it just steals your vision while you’re scrolling TikTok. I got mine caught early because I asked for my retinal images after every visit. Now I’ve got a little album of my retina’s journey. Weird? Maybe. Lifesaving? Absolutely.
/p>HOW IS THIS EVEN A CONVERSATION? Someone let their HbA1c hit 8.5 and they got pushed to biennial screening? That’s not risk-based that’s negligence. I had a friend go blind in one eye because her doctor trusted the algorithm over her numbers. Don’t be that person. If your sugar’s up, you get seen. No excuses. No ‘but it’s expensive’-blindness is more expensive.
/p>STOP WAITING. If you have diabetes and you haven’t had a retinal scan in 12 months you’re playing Russian roulette with your sight. I’m not here to be nice. I’m here to save your vision. Get. The. Scan. Now. Your future self will thank you. Or cry. Probably cry.
/p>I’ve been living with type 2 for 18 years and I’ve had zero retinopathy because I treat it like a full-time job not a side hobby. I track my sugars like a stock portfolio I check my BP weekly I quit smoking cold turkey in 2020 and I got my kidneys checked last month. The eye doc said I’m low risk so I go every 2 years. But here’s the thing I don’t just trust the schedule I trust the data. If my HbA1c jumps I call the office immediately. It’s not about the calendar it’s about the trend. And if you’re not doing that you’re gambling with your eyes.
Also I’ve been using the D-Eye app with my phone adapter since last year. It’s not perfect but it’s way better than nothing. I take a pic every month and send it to my endo. He says it’s helping him catch early changes. No more waiting for the ‘annual’ to show something’s wrong.
And yeah I know some people say AI can’t replace a doctor. But when you live in a rural town with no ophthalmologist within 100 miles AI is the only reason I’m not blind right now. It’s a tool not a replacement. Use it. Embrace it. Don’t fear it.
And if you think laser treatment is scary I got mine done in 2018. Felt like someone shined a flashlight in my eye while a drum beat in my head. No pain. No tears. Just a few hours of light sensitivity. And now I can still read the license plate on the car in front of me at night. That’s worth it.
Also don’t let anyone tell you insulin means you’re doomed. I’m on basal-bolus and I’ve had cleaner retinas than half the non-insulin users I know. It’s not about the meds it’s about the management. Consistency beats intensity every time.
And for the love of all that’s holy stop saying ‘I can’t afford it.’ There are free screenings everywhere. Community clinics. Pharmacies. Mobile vans. Even Walmart does them for $25. If you can afford a new phone you can afford to protect your sight. That’s not an option that’s a requirement.
And if you’re pregnant? Monthly scans. No debate. Your body is changing. Your eyes are changing. Don’t wait. Don’t hope. Don’t assume. Just go. I’ve seen too many cases where women lost vision after delivery because they skipped the postpartum check. It’s not rare. It’s preventable.
And one last thing: if your doc says ‘you’re low risk’ and you’ve got a history of wild glucose swings even if your current number looks good-you’re still high risk. Stability matters more than the number on the screen. That’s the truth nobody tells you.
/p>Man this hits different when you’ve seen your cousin lose both eyes because he thought ‘it won’t happen to me’ 🌅 In India we got these mobile retinal vans rolling through villages now-no fancy clinics just a guy with a phone adapter and a tablet. He takes pics while you’re waiting for your sugar test. Within 20 mins you know if you’re safe or not. No waiting. No bureaucracy. Just tech doing what it’s supposed to. If you’re reading this and you’re in a place with no eye doctors-don’t wait. Find the van. Find the app. Find the help. Your eyes are your most expensive asset. Don’t let them go dark because you were too lazy to click a button.
/p>Just got my 2-year screening today-no retinopathy! 🥹 So relieved. Thanks for the reminder to track my images. I’m keeping them all now. ❤️
/p>The article incorrectly states that AI can detect retinopathy with 94.5% accuracy. That figure refers to sensitivity for referable disease-not overall diagnostic accuracy. The specificity is lower. Also, the term ‘AI-powered tools’ is misleading. These are algorithmic image classifiers, not artificial intelligences. And Google DeepMind never developed a standalone diagnostic tool for retinopathy-it was a research prototype. Please correct this misinformation before it spreads.
/p>If you're not monitoring your eGFR and serum creatinine alongside your HbA1c you're not managing diabetes you're just winging it. Retinopathy is a microvascular complication not a standalone event. You need systemic control. No one talks about the renin-angiotensin-aldosterone axis but if your RAS is dysregulated your retinal endothelium is toast. And if your LDL is above 100 forget about laser or anti-VEGF-it’s not the treatment that’s failing it’s your metabolic profile. Fix the root not the symptom.
/p>I used to dread my eye appointments. Now I look forward to them. It’s the one time I feel like someone is really looking out for me. My doc shows me the pictures every time. I even printed one and taped it to my fridge. A little reminder to eat the broccoli. 😊
/p>my doc said i can wait 2 years but my sugar been kinda up lately so i just went anyway lol. no drama just a lil blurry vision after the drops. but good news-no damage! so maybe i’ll go every 18 months now? 🤷♀️
/p>