
When older adults take medications, their kidneys don’t work the same way they did at 30. That’s not just a minor detail-it’s the difference between safe treatment and serious harm. About 30% of common drugs prescribed to seniors are cleared almost entirely by the kidneys. If kidney function is misjudged, even slightly, those drugs can build up to toxic levels. A 75-year-old with normal creatinine levels might actually have kidney function at half what it was at age 40. And if their doctor uses the wrong formula to estimate it, they could be getting a dangerous dose.
Why Kidney Function Changes with Age
Your kidneys don’t just slow down with age-they shrink, get less blood flow, and lose filtering units called nephrons. By age 70, average kidney filtration (eGFR) drops from 116 mL/min/1.73 m² in young adults to about 75 mL/min/1.73 m². That’s not disease. That’s normal aging. But many doctors treat it like disease. They see a lower eGFR and assume kidney damage, when it’s just aging. This leads to under-dosing or stopping useful medications like blood pressure pills or statins, which can be just as harmful as over-dosing.
Here’s the real problem: most drug labels still say “adjust dose if eGFR is below 60.” But if you’re 82 and your eGFR is 58 because of aging-not kidney disease-you might be denied a life-saving drug. Or worse, you might get the full dose because your doctor used a formula that overestimates your kidney function.
The Equations That Matter (and Which Ones to Avoid)
There are three main equations used to estimate kidney function. Each has strengths and blind spots, especially in seniors.
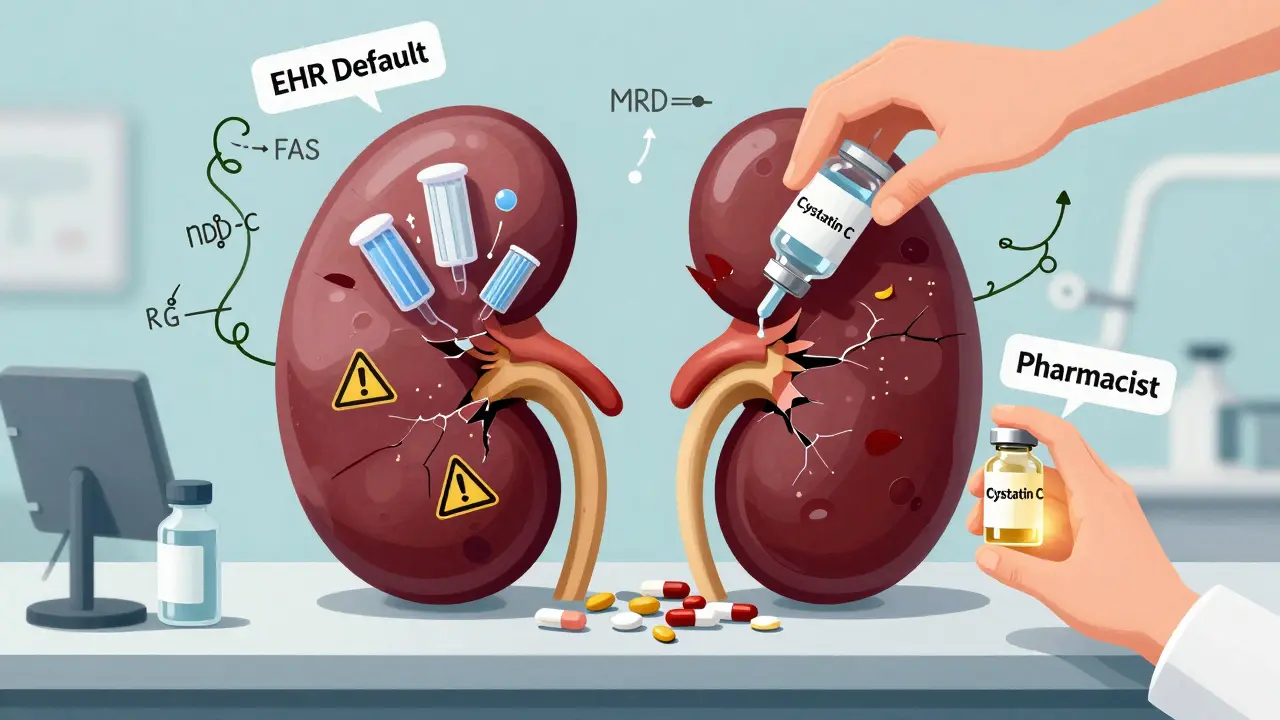
- Cockcroft-Gault (CG): Developed in 1976. Uses age, weight, gender, and serum creatinine. It estimates creatinine clearance, not GFR. It’s old, but it still works well-if you use ideal body weight. Many EHRs automatically use actual body weight, which gives wrong results for both thin and obese seniors. Studies show using ideal body weight cuts dosing errors by 25% in older adults.
- MDRD: Created in 1999. Better than CG for estimating GFR, but it’s biased upward in seniors. It often says kidney function is better than it really is. In patients over 65, it overestimates by about 1.4 mL/min/1.73 m². That might sound small, but for a drug like warfarin or digoxin, that’s enough to cause toxicity.
- CKD-EPI: Launched in 2009. Now the most common in hospitals. It’s more accurate than MDRD for people with mild kidney disease. But in seniors over 75, especially those who are frail or underweight, it still misclassifies up to 30% of patients. It often puts them in a lower kidney disease stage than they’re actually in.
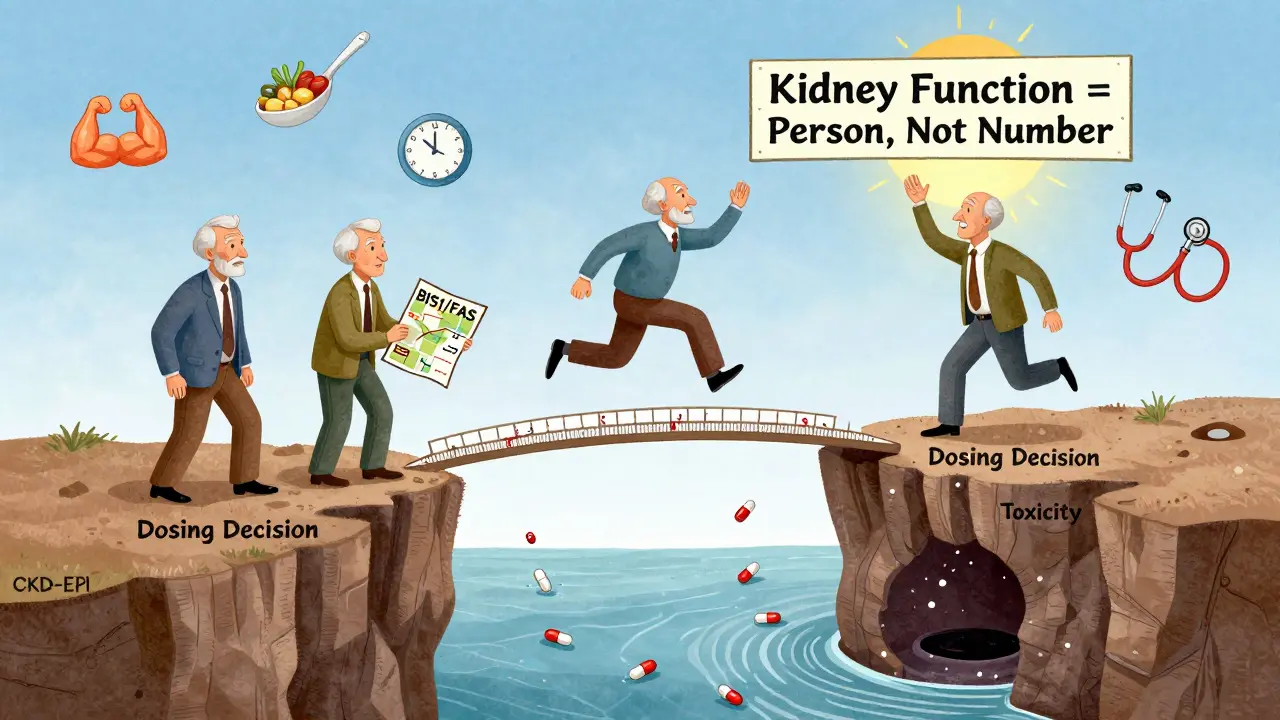
For seniors over 75, especially those with low muscle mass, malnutrition, or chronic illness, two newer equations are far more accurate:
- BIS1: Developed by German researchers. Designed specifically for very old adults. In one study of 85-year-olds, BIS1 was accurate within 30% of the true value in 95% of cases. CKD-EPI only hit that mark in 78%.
- FAS (Full Age Spectrum): Works across all ages, but shines in the elderly. It’s less variable and more precise than CKD-EPI in patients over 70.
Here’s the catch: most electronic health records still default to CKD-EPI. If you’re a pharmacist or clinician, you’re often stuck with what the system gives you. That’s why 63% of pharmacists in senior care say they override EHR recommendations at least once a week.
When to Use Cystatin C
Serum creatinine is the standard marker. But it’s flawed. Creatinine comes from muscle. A frail 80-year-old with low muscle mass might have a normal creatinine level-even though their kidneys are failing. That’s a false negative. Enter cystatin C. It’s a protein made by all cells, not just muscle. It’s not affected by body size or diet. It’s a better marker for true kidney function in thin, frail, or malnourished seniors.
Cystatin C tests cost $50-$75 more than creatinine. But in patients with borderline eGFR (45-59 mL/min/1.73 m²) and no signs of kidney damage (like protein in urine), a cystatin C test can clarify whether the low eGFR is real or just a muscle issue. If cystatin C is normal, you can safely give full doses of medications. If it’s high, you know the kidneys are truly impaired.
Real-World Mistakes and Fixes
One 88-year-old woman in a nursing home was on vancomycin for a skin infection. Her EHR showed eGFR of 62 using CKD-EPI. Full dose given. She developed kidney failure and confusion. Her doctor switched to BIS1. The new eGFR was 38. Dose halved. She recovered. No more toxicity.
Another case: a 79-year-old man on rivaroxaban for atrial fibrillation. His creatinine was 1.1 mg/dL. CKD-EPI said eGFR was 59. He got the full dose. He bled internally. Cystatin C testing revealed true eGFR was 41. He was switched to a lower dose and stabilized.
These aren’t rare. They’re routine. A 2023 study found that 38% of dosing errors in seniors came from using Cockcroft-Gault with actual body weight instead of ideal body weight. That’s not ignorance. That’s system design. Most EHRs don’t even let you choose.
What Should You Do?
If you’re managing medications for a senior, here’s your practical checklist:
- Check the equation used. Ask: “Is this CKD-EPI, MDRD, or Cockcroft-Gault?” If it’s CG, confirm if it’s using ideal body weight, not actual weight.
- For seniors over 75, especially if frail or thin, request BIS1 or FAS. These are not experimental. They’re evidence-based. The American Society of Nephrology recommends them for this group.
- Use cystatin C if eGFR is between 45-59 and there’s no protein in urine. It tells you if the kidney is truly slow or if it’s just low muscle mass.
- Don’t trust one number. Kidney function changes daily. If a senior is sick, dehydrated, or has just started a new drug, recheck in 3-5 days.
- Know the drug’s requirements. Drugs like dabigatran, rivaroxaban, aminoglycosides, and metformin need precise dosing. Check if the drug handbook includes dosing guidance for BIS1 or cystatin C. Most don’t. That’s why you need to dig deeper.
Tools and Resources
You don’t have to guess. There are free, reliable tools:
- National Kidney Foundation eGFR Calculator (updated Nov 2023): Lets you plug in creatinine, age, sex, race, and choose equation.
- American Geriatrics Society’s “Kidney Function Assessment in Older Adults” Toolkit (Jan 2024): Downloadable PDF with dosing tables, equation selection flowcharts, and case examples.
- Epic Systems (EHR): Since 2022, it auto-selects BIS1 for patients over 75. If your clinic uses Epic, check if it’s turned on.
Even with these tools, the biggest barrier isn’t knowledge-it’s access. Most community clinics still use default CKD-EPI. It takes a pharmacist, nurse, or concerned family member to push for the right calculation.
The Future: Personalized, Not One-Size-Fits-All
The field is moving fast. In 2024, a new equation called CKD2024 was introduced. It combines creatinine and cystatin C with age-specific math. Early results show 15% better accuracy in people over 80. The National Institute on Aging is funding a $4.2 million project to build point-of-care kidney tests that adjust for muscle mass and nutrition.
But the biggest shift isn’t technical. It’s cultural. We’re moving away from “one equation fits all” to “which equation fits this person?” A 90-year-old who’s 90 pounds and eats little needs a different approach than a 70-year-old who’s strong and active. The same drug, same creatinine, same age-different kidneys.
And that’s the key: kidney function isn’t a number on a chart. It’s a reflection of a person’s body, their muscle, their food, their illness, their age. The best monitor isn’t a lab test. It’s a thoughtful, informed clinician who asks: ‘Does this make sense for her?’
What’s the best equation for a frail 80-year-old with low muscle mass?
For a frail senior over 75 with low muscle mass, the BIS1 or FAS equation is the most accurate. These were designed specifically for older adults and avoid the overestimation common with CKD-EPI or MDRD. If creatinine is normal but the person is thin or malnourished, also consider a cystatin C test to confirm true kidney function.
Why can’t we just use serum creatinine alone?
Serum creatinine alone is misleading in seniors because it reflects muscle mass, not kidney function. A thin 85-year-old may have low creatinine even with severe kidney impairment. A muscular 70-year-old may have high creatinine but normal kidneys. That’s why we need equations that adjust for age, weight, and gender-and sometimes cystatin C.
Should I use ideal body weight or actual body weight in Cockcroft-Gault?
Always use ideal body weight (IBW) for Cockcroft-Gault in seniors. Actual body weight overestimates kidney function in obese patients and underestimates it in those who are underweight. Studies show using IBW reduces dosing errors by 25% in older adults. Many EHRs default to actual weight-this is a common source of dangerous mistakes.
Is cystatin C testing worth the extra cost?
Yes, if the patient is over 75, has borderline eGFR (45-59 mL/min/1.73 m²), and no signs of kidney disease like protein in urine. Cystatin C can prevent unnecessary dose reductions or dangerous overdoses. The cost is $50-$75, but the cost of a medication overdose can be hospitalization, permanent kidney damage, or death.
What should I do if my EHR only shows CKD-EPI?
Don’t accept it. Use the National Kidney Foundation’s online calculator or the American Geriatrics Society toolkit to recalculate using BIS1 or CG with ideal body weight. If you’re a pharmacist or clinician, advocate for changing your clinic’s defaults. Many institutions now allow manual override. For critical drugs like anticoagulants or antibiotics, it’s not optional-it’s essential.
Next Steps
If you’re a caregiver, ask your pharmacist or doctor: “Which equation are you using to calculate my loved one’s kidney function?” If they don’t know, ask them to check. If you’re a clinician, download the American Geriatrics Society toolkit. Run a BIS1 calculation on your next frail senior patient. Compare it to CKD-EPI. You might be surprised. And if you’re a pharmacy system designer-stop defaulting to CKD-EPI for everyone. Build in age-based logic. Let the system adapt to the person, not the other way around.





