Probiotic Safety Risk Assessment
Probiotic Safety Assessment
This tool helps assess your personal risk of probiotic-related infections based on your medical condition, medications, and immune status. Always consult your healthcare team before making decisions about probiotics.
When you're on immunosuppressants-whether for a transplant, autoimmune disease, or cancer treatment-your body is already playing defense. Every extra germ, every unfamiliar microbe, becomes a potential threat. So when someone suggests taking probiotics to help with digestion or gut health, it sounds harmless. But here’s the catch: probiotics aren’t just harmless bacteria. In people with weakened immune systems, they can turn dangerous.
What Happens When Probiotics Meet Immunosuppressants?
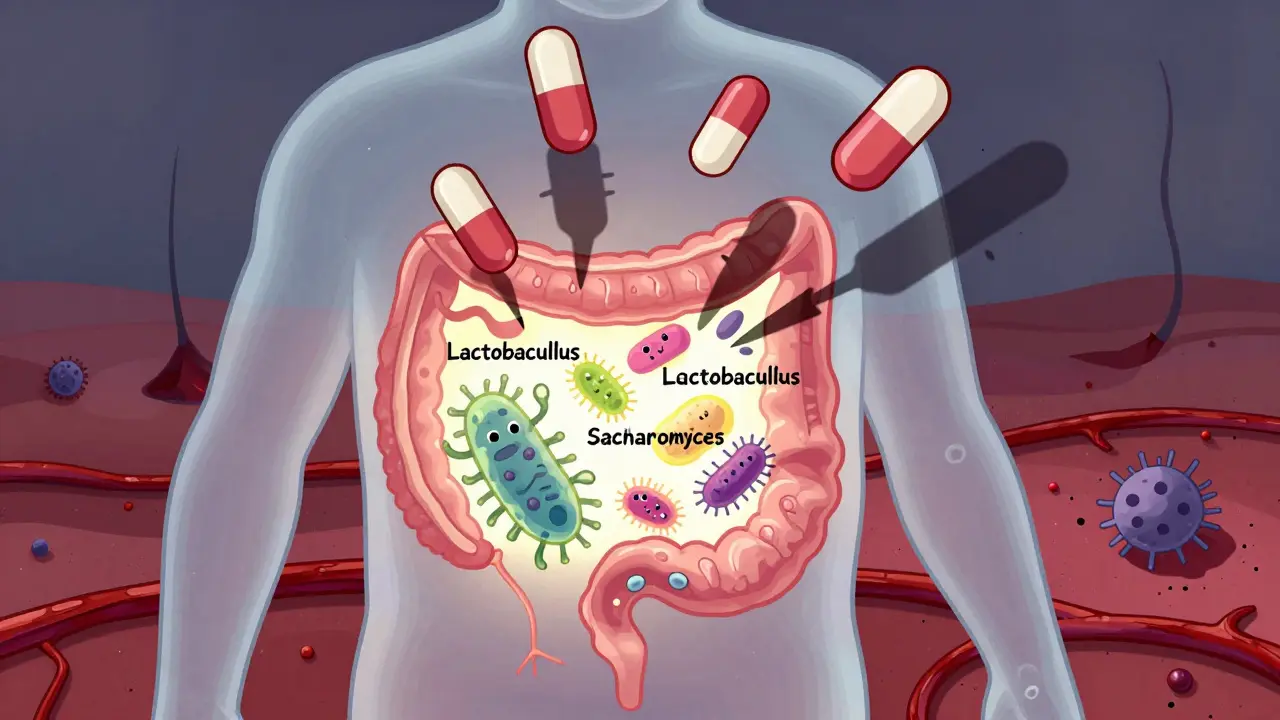
Probiotics are live microbes-mostly bacteria like Lactobacillus and Bifidobacterium, or yeast like Saccharomyces boulardii. In healthy people, they help balance gut flora, fight off bad bacteria, and even support immunity. But in someone taking drugs like cyclosporine, tacrolimus, mycophenolate, or prednisone, those same microbes can slip through the gut lining and enter the bloodstream. This isn’t theoretical. Between 2000 and 2020, 47 documented cases of probiotic-related infections occurred in immunocompromised patients. Over 80% of those cases happened in people on immunosuppressants. The most common culprits? Lactobacillus rhamnosus GG and Saccharomyces boulardii. Infections included bloodstream infections, heart valve infections, and even pancreatitis. Some were fatal.Who’s at the Highest Risk?
Not everyone on immunosuppressants is equally at risk. The danger depends on how weak your immune system is and what kind of drugs you’re taking.- Neutropenia (ANC <500 cells/µL): If your white blood cell count is this low-common during chemotherapy-your body can’t fight off even friendly microbes. Probiotics are strictly avoided here.
- Central venous catheters: Patients with lines in their chest or neck for IV meds or nutrition have a 27% higher risk of infection from Saccharomyces boulardii. The yeast can cling to the catheter and grow right into the bloodstream.
- Recent organ transplant: Especially in the first 3 months after transplant, immunosuppression is at its peak. Studies show this group has a higher chance of developing probiotic-related sepsis.
- Stem cell transplant: Bone marrow recipients face a 4.2-fold increased risk of bacteremia when using probiotics.
- HIV with CD4 <100: Those with very low T-cell counts are at 3.8 times higher risk of fungal infections from probiotics.
Who Might Be Safe? It’s Not Black and White
There are exceptions. Not every immunosuppressed person needs to avoid probiotics entirely.- Liver transplant recipients: A 2022 meta-analysis found probiotics actually reduced bacterial infections by 34% with no increase in serious side effects. This is the only group with strong evidence of benefit.
- Stable autoimmune patients on one drug: Someone on low-dose methotrexate with no recent infections or hospitalizations might tolerate specific strains under supervision.
- HIV with CD4 >200: Risk is minimal here, but caution still applies.
Not All Probiotics Are Created Equal
The strain matters more than the brand. Lactobacillus rhamnosus GG is the most common strain in commercial products-and also the most frequently linked to infections. Saccharomyces boulardii, a yeast, is especially risky with catheters. One 2022 study showed single-strain probiotics had 63% lower risk of translocation than multi-strain blends. Many over-the-counter supplements contain 10-15 different strains. That’s a red flag for immunosuppressed patients. If probiotics are considered at all, doctors recommend sticking to one well-studied strain with documented safety data.What Do Experts Actually Recommend?
Guidelines vary, but the safest approach is risk-based. The Infectious Diseases Society of America (IDSA) 2023 guidance breaks patients into four categories:- Category 1 (Highest Risk): Neutropenia, recent stem cell transplant, central lines → Absolute contraindication. No probiotics.
- Category 2 (Moderate Risk): Solid organ transplant within 3 months, multiple immunosuppressants → Only use after infectious disease consultation.
- Category 3 (Lower Risk): Stable autoimmune disease on one drug, CD4 >200 → Selective strains only, under supervision.
- Category 4 (Low Risk): No immunosuppression → Standard use is fine.
What About the People Who Say It Worked for Them?
You’ll find stories online. Someone on methotrexate for rheumatoid arthritis says probiotics helped their bloating. Another person claims they’ve taken them for years after a kidney transplant with no issues. Those stories are real-but they’re anecdotes. They don’t replace data. A 2022 survey of 1,247 autoimmune patients found 68% reported improved digestion with probiotics. But here’s what that survey didn’t measure: Did they have low white blood cells? Were they on multiple drugs? Did they develop a fever? Were they monitored for infection? One patient’s good outcome doesn’t mean it’s safe for everyone. In medicine, we don’t treat based on stories-we treat based on patterns. And the pattern is clear: when immunosuppressed people take probiotics, infections happen.
What Should You Do?
If you’re on immunosuppressants:- Don’t start probiotics on your own. Even if your doctor didn’t mention it, don’t assume it’s safe.
- Ask your doctor or pharmacist: "Is my immune system currently too weak for probiotics?" Be specific about your meds and lab values.
- If probiotics are approved: Use only one strain. Avoid Saccharomyces boulardii entirely if you have a central line. Make sure you know the exact strain name (e.g., Lactobacillus rhamnosus GG ATCC 53103).
- Watch for symptoms: Fever over 38.3°C (101°F), chills, or unexplained fatigue while taking probiotics? Stop immediately and get blood cultures.
- Document everything: If you’re given the green light, keep a record of the product name, strain, dose, and date started.
What’s Coming Next?
Science is moving toward safer alternatives. Researchers are testing postbiotics-inactivated microbes and their metabolic byproducts. These offer immune benefits without the risk of live organisms causing infection. Early trials show promise: a phase 2 trial found a 40% reduction in C. difficile infections in immunocompromised patients with zero adverse events. Also, the PROTECT registry-launched in 2023-is tracking 5,000 immunosuppressed patients across 47 centers. Results are expected in 2025 and could finally give us clear, evidence-based rules instead of guesswork.Bottom Line
Probiotics aren’t evil. For most people, they’re helpful. But for those on immunosuppressants, they’re a gamble with serious stakes. The risk isn’t just infection-it’s sepsis, organ failure, or death. The safest choice? Don’t take them unless your care team explicitly says it’s okay, and even then, use only one strain and monitor closely. If you’re unsure, talk to your doctor. Bring this article. Ask: "Based on my meds and my immune status, is this safe?" That’s the only question that matters.Can I take probiotics if I’m on prednisone?
It depends on your dose and overall immune status. Low-dose prednisone (5 mg or less daily) for stable conditions like asthma or arthritis may be okay with medical approval. But if you’re on higher doses, have other immunosuppressants, or have had recent infections, probiotics are risky. Always check with your doctor before starting.
Are probiotics safe after a kidney transplant?
Generally, no-especially in the first 3 months. Your immune system is suppressed to prevent rejection, and that’s when you’re most vulnerable. Case reports show probiotics have triggered bloodstream infections in kidney transplant patients. Even if you feel fine, your body can’t fight off these microbes. Wait until your transplant team says it’s safe, and even then, only use one strain under supervision.
What probiotic strains are safest for immunosuppressed patients?
There’s no universally safe strain for immunosuppressed people. But if a probiotic is approved by your doctor, Lactobacillus rhamnosus GG (ATCC 53103) has the most safety data. Avoid Saccharomyces boulardii entirely if you have a central line or low white blood cell count. Multi-strain products are riskier than single-strain ones. Always ask for the exact strain name and lot number.
Do probiotics interfere with immunosuppressant drugs?
Probiotics don’t directly interfere with how immunosuppressants work in your body. The problem isn’t drug interaction-it’s infection risk. The microbes in probiotics can cross into your bloodstream when your immune system can’t stop them. That’s what causes sepsis, not a chemical reaction with your meds.
Can I take probiotics during chemotherapy?
No-not during periods of myelosuppression, when your white blood cell count drops below 1,000 cells/µL. At 87% of U.S. cancer centers, patients are explicitly told to avoid probiotics during chemotherapy. The risk of bacterial or fungal infection is too high. Wait until your counts recover and your oncologist gives the green light.
Are there alternatives to probiotics for gut health on immunosuppressants?
Yes. Focus on diet: fiber-rich foods like oats, beans, and vegetables feed your good gut bacteria naturally. Stay hydrated. Avoid processed sugars and artificial sweeteners that disrupt gut balance. Some doctors recommend prebiotics (like inulin or resistant starch) or postbiotics, which are non-living microbial compounds. Postbiotics are being studied as a safer alternative because they don’t carry live microbes.






12 Comments
As someone who’s been on immunosuppressants for five years after a kidney transplant, I can’t stress this enough: never just start a probiotic because a friend said it helped their digestion. I almost ended up in the ICU last year because I took a ‘natural’ gut supplement. Turned out it had Saccharomyces boulardii. Fever, chills, blood cultures positive-it was terrifying. My doctor said I got lucky. Don’t be like me.
/p>okay so i just read this and i’m like… wait so all those gummies i’ve been taking for ‘gut health’ are basically tiny time bombs?? 😳 i thought probiotics were like… good bacteria?? like, the kind that don’t hurt you?? this is wild. i’m deleting my cart right now. no more ‘immune support’ nonsense.
/p>Let me be blunt: if you’re on immunosuppressants and you’re casually popping probiotics because you saw a TikTok influencer say they ‘fixed their bloating,’ you’re playing Russian roulette with your life. I’ve seen patients die from this. Not because they were weak. Not because they didn’t try hard enough. Because someone told them it was ‘natural’ and therefore safe. It’s not. It’s a Trojan horse. Stop trusting influencers. Start trusting your transplant team.
/p>Isn’t it ironic? We spend our lives trying to ‘balance’ our microbiomes, to ‘coexist’ with the unseen world within us-yet when our defenses falter, the very organisms we once welcomed become our executioners? The body is not a garden you can prune with a spoonful of yogurt. It is a cathedral of delicate equilibrium, and when the walls are breached by even the most benevolent of microbes, the sacred silence shatters. We are not enemies of nature-we are its fragile guests. And when the guest is weak, the host must be cautious. Probiotics are not evil. They are indifferent. And indifference, in a body under siege, is deadly.
/p>Why do we keep treating immunosuppressed patients like they’re just ‘a little more sensitive’? This isn’t ‘maybe be careful.’ This is a medical emergency waiting to happen. If your doctor hasn’t explicitly warned you about probiotics, they’re not doing their job. Period. Stop normalizing risk. Stop letting supplement companies profit off ignorance. This is a public health blind spot, and it needs to be addressed-NOW.
/p>So if I’m on low-dose prednisone for my asthma and I feel fine… is it totally off-limits? Or is there a gray area? I don’t wanna be reckless, but I also don’t wanna miss out on something that might help my digestion. What’s the line between being safe and being paranoid?
/p>Western medicine always overreacts. In India, we’ve used curd and fermented foods for centuries. No one dies from probiotics. You people are scared of everything. This is just Big Pharma pushing pills instead of food. You think your ‘studies’ are better than generations of tradition? I’m not stopping my daily yogurt. My immune system is stronger than your fear.
/p>My mom’s on tacrolimus after her liver transplant. She’s been taking L. rhamnosus GG for two years now. No issues. Her doctor approved it. She’s got stable labs, no catheters, no other meds. This article says it’s possible. Maybe it’s not a blanket ‘no’-maybe it’s about context?
/p>Probiotics are the placebo of the wellness industry-a glittery bandage on a gaping wound. We want to believe in quick fixes, in tiny living things that fix everything, because the truth is too heavy: our bodies are fragile, our systems are complex, and no capsule can replace the discipline of sleep, of food, of quiet. We’ve outsourced healing to a pill, and now we’re paying the price in sepsis and ICU beds. Maybe the real probiotic is stillness. Maybe the real prebiotic is patience.
/p>Postbiotics are the future. No live organisms. No translocation risk. Just microbial metabolites-SCFAs, bacteriocins, enzymes-that modulate immunity without infection potential. Phase 2 data looks strong. Ask your GI about butyrate supplements or heat-killed strains. Safer. Science-backed. No FDA warnings. This is where we’re headed.
/p>So let me get this straight… if I’m on immunosuppressants, I can’t take probiotics… but I can eat kimchi? Or sauerkraut? Or yogurt? Are those ‘natural’ versions somehow magically safer? Or is this just another case of ‘pharma says no, but food is fine’? Because if I’m eating a fermented food with live cultures, isn’t that the same thing? Someone explain this to me before I start questioning everything I eat.
/p>My brother’s a transplant patient. He’s been on this list for years. I showed him this article. He said, ‘I’ve been taking LGG for 4 years. No fever. No infection. My doctor knows.’ He’s not reckless-he’s informed. Maybe the real problem isn’t probiotics. It’s that we treat every immunosuppressed person like they’re the same. We need nuance. Not fear. Not blanket bans. Just good, careful, individualized care.
/p>