
When you’re on a brand-name medication that costs $2,000 a month, even with insurance, your out-of-pocket bill can feel impossible. That’s where manufacturer copay assistance cards come in. These aren’t discounts or coupons you find in a magazine. They’re financial tools built into the system to help people with private insurance afford expensive drugs. But using them wrong can leave you with a huge bill later. Here’s how to actually use them - and what to watch out for.
What Are Manufacturer Copay Assistance Cards?
These cards are offered directly by drug makers like AbbVie, Pfizer, or Roche. They’re designed for people with commercial health insurance - not Medicare, Medicaid, or no insurance at all. The card works like a coupon: when you fill your prescription, the pharmacy swipes it along with your insurance. The manufacturer then pays part or all of your copay or coinsurance. For example, if your medication costs $2,000 and your insurance says you owe $500, the card might cover $450 of that. You pay $50. Sounds great, right? But there’s a catch. The card only works if your drug doesn’t have a generic version, and it’s usually for high-cost specialty medications like those for rheumatoid arthritis, multiple sclerosis, or cancer.How Do You Get One?
You don’t get these cards from your doctor’s office. You have to go to the drug manufacturer’s website. Search for your exact medication - not just the class of drug. If a card is available, you’ll see a link to apply. You’ll need:- Your insurance card
- Proof of income (sometimes)
- Your doctor’s name and prescription number
How to Use It at the Pharmacy
Bring the card with you when you pick up your prescription. Tell the pharmacist you’re using a manufacturer copay card. They’ll enter the card number into their system along with your insurance info. The pharmacy then sends a claim to the manufacturer, who pays their portion. You pay the rest. It’s automatic. You don’t have to submit receipts or wait for reimbursement. The discount shows up right at the counter.The Hidden Problem: Copay Accumulator Programs
Here’s where things get dangerous. Many insurance plans now use what’s called a copay accumulator program. This means the money the manufacturer pays doesn’t count toward your deductible or out-of-pocket maximum. Think of it this way: you’re paying $0 for six months because the card covers everything. You think you’re making progress toward hitting your $7,000 out-of-pocket cap. But under an accumulator program, that $12,000 the manufacturer paid? It doesn’t count. When the card runs out - maybe after $8,000 in total assistance - you suddenly owe the full $2,000 monthly cost. And you’re still at $0 toward your deductible. You might owe $7,000 more before your insurance even kicks in. Studies show about 70% of commercial insurance plans in the U.S. use these programs as of 2023. That means most people using copay cards are at risk of a financial shock later in the year.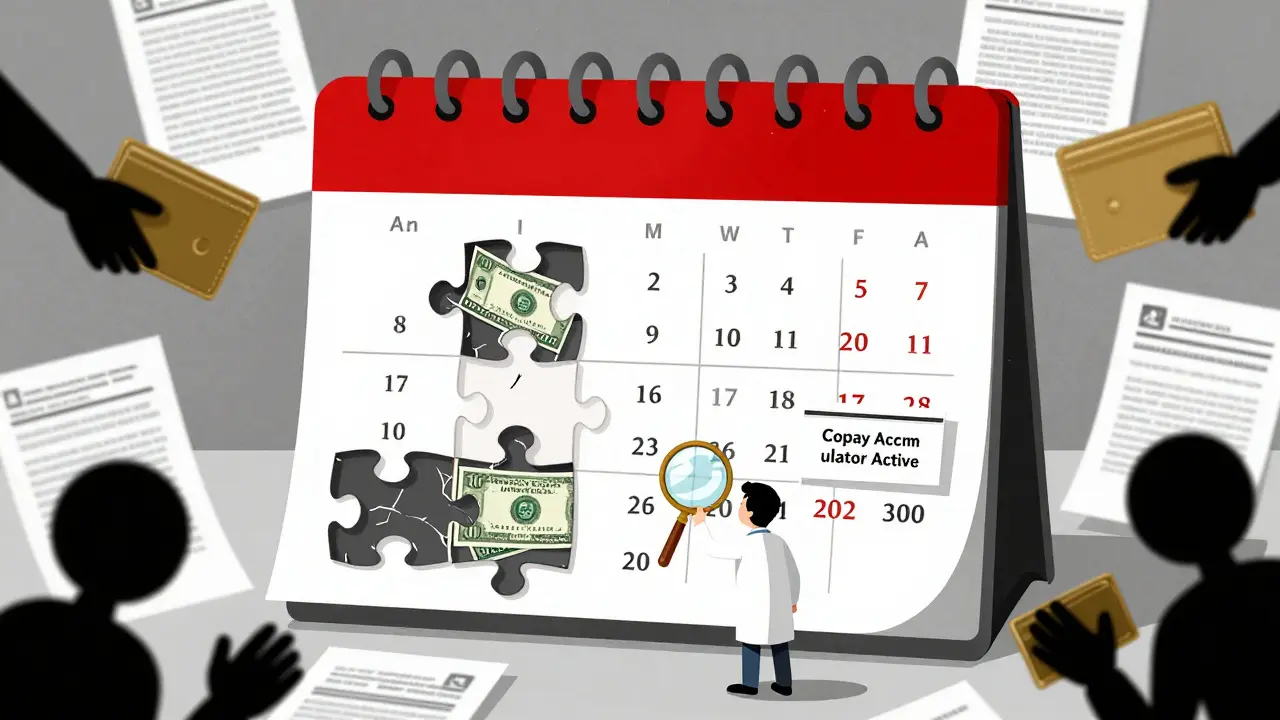
Copay Maximizer vs. Copay Accumulator
Not all programs are the same. Some insurers use a copay maximizer. This one spreads the manufacturer’s contribution evenly over the year. So if your card gives you $8,000 and your monthly copay is $2,000, the plan treats it as if you paid $2,000 each month - even though you paid $0. That means your out-of-pocket costs are counted, and you’ll hit your cap faster. But if your plan uses an accumulator, the manufacturer’s payment is ignored. You pay nothing now - but you’re still far from your cap. When the card expires, you’re stuck with the full cost. You need to know which one your plan uses. Call your insurer. Ask: “Do you use a copay accumulator or maximizer program?” Don’t assume. Don’t rely on your pharmacy to know. They often don’t.What About Medicare or Uninsured Patients?
If you’re on Medicare Part D, you cannot use these cards. Federal law bans manufacturers from subsidizing government-funded prescriptions. That’s why you’ll see a note on every card: “Not valid for Medicare or Medicaid.” If you’re uninsured, these cards won’t help either. But you might qualify for a different kind of help: patient assistance programs (PAPs). These are run by the same manufacturers but are meant for low-income or uninsured people. They’re not the same as copay cards. PAPs often give you free medication for a year. You can find them on the same manufacturer website - look for “Patient Assistance Program” or “Uninsured Support.”Alternatives: Pharmacy Discount Cards
If you’re on Medicare, uninsured, or your plan uses an accumulator, try a pharmacy discount card like GoodRx or SingleCare. These aren’t tied to insurance. They negotiate cash prices with pharmacies. You can use them for generics or brand-name drugs - even if you have insurance. Sometimes, the cash price with a discount card is lower than your insurance copay. Always compare. Enter your drug, dose, and pharmacy into GoodRx. See what the cash price is. Then see what your copay would be with your card. Choose the cheaper option.
What to Do Before Your Card Runs Out
If you’re using a copay card, track it. Write down:- Your monthly copay cost
- Your card’s annual limit (often $8,000)
- How many months you’ve used it
State Laws Are Starting to Change Things
Some states are pushing back. California passed a law in 2021 requiring insurers to count manufacturer payments toward out-of-pocket maximums. New York and Illinois have similar rules. But not all states do. And even in those states, some plans are still finding ways around it. It’s a patchwork. That’s why you can’t rely on location. You still have to ask your insurer: “Do you count copay assistance toward my deductible?”Final Tips
- Never use a copay card if you’re on Medicare - it’s illegal and can get your doctor in trouble.
- Always compare the card’s savings to a GoodRx cash price.
- Call your insurer every January to confirm your plan’s accumulator policy - they can change yearly.
- Keep a copy of your card, your annual limit, and your monthly usage in a folder or digital note.
- Ask your pharmacist if they know your plan’s policy. If they don’t, ask for the pharmacy benefits manager’s phone number.






14 Comments
So let me get this straight-you’re telling me I can pay $0 for six months, then suddenly owe $7,000 out of nowhere because some insurance exec decided ‘helping people’ means ‘helping them go bankrupt later’? 🤡
/p>i just got my card for my rheumatoid arthritis med last month and i had no idea about the accumulator thing. i called my insurer today and they said ‘oh yeah we do that’ like it was normal. i’m freaked out. thanks for the heads up.
/p>Let’s be real-the entire pharmaceutical-industrial complex is a rigged casino. These copay cards? They’re not charity. They’re a bait-and-switch engineered by Big Pharma to keep you hooked while insurers dodge financial responsibility. You think they care about your health? No. They care about your loyalty. Your addiction. Your $2,000 monthly habit. And now, with the accumulators, they’ve turned your desperation into a spreadsheet. You’re not a patient-you’re a revenue stream with a pulse. And when the card expires? You’ll be begging for a PAP while your kidneys fail. This isn’t healthcare. It’s predatory capitalism with a pretty logo.
/p>GoodRx saved me last month. My copay was $180. Cash price with discount was $95. No card needed.
/p>How quaint. You’ve managed to distill an entire systemic failure into a ‘tip’-as if the problem were merely one of user ignorance, rather than a grotesque, profit-driven architecture designed to extract maximum value from the sick. The fact that you’re still surprised by this? That’s not ignorance. That’s complicity.
And yet, you’ll probably still use the card. Because you’re not a revolutionary-you’re a rational actor in a broken system. You’re not trying to fix it. You’re just trying not to die before your deductible resets.
How tragic. How… bourgeois.
Meanwhile, in India, we don’t have ‘copay cards.’ We have family pooling. We have barter. We have walking five kilometers to a clinic that gives medicine for free because the government doesn’t care, but the community does. You call this ‘healthcare’? This is a corporate loyalty program with a stethoscope.
At least in Mumbai, no one pretends the system is fair. Here? You’re told to ‘play smart’ while the house burns down around you.
And you wonder why we’re all so angry.
/p>Oh please. You think this is bad? Try being on insulin in rural Tennessee without insurance. You don’t get ‘cards.’ You get a choice between dialysis and dinner. The ‘system’ isn’t broken-it’s working exactly as intended. The only people who don’t understand this are the ones who still believe in ‘fairness’ and ‘insurance.’
Also, GoodRx? That’s just another middleman siphoning off your dignity. The real solution? Nationalize drug pricing. But no, let’s keep letting CEOs buy yachts while you ration pills.
Pathetic.
/p>For those unfamiliar with the terminology: copay accumulator programs (CAPs) are a form of cost-shifting mechanism wherein third-party payments (e.g., manufacturer coupons) are excluded from the calculation of the patient’s annual out-of-pocket maximum (OOPM). This effectively nullifies the therapeutic benefit of the coupon, as the patient remains financially vulnerable even after substantial expenditure. The legal basis for CAPs stems from the ambiguity in the Affordable Care Act’s definition of ‘out-of-pocket costs,’ which does not explicitly require inclusion of third-party payments. As of 2023, approximately 70% of commercial plans in the U.S. employ CAPs, per the Kaiser Family Foundation. Mitigation strategies include: (1) proactive verification of plan design via PBMs, (2) utilization of patient assistance programs (PAPs) as a bridge, and (3) advocacy for state-level legislation (e.g., CA SB 186) mandating inclusion of manufacturer contributions in OOPM tracking.
/p>I just want to say thank you for writing this. I’ve been using a copay card for my MS med for two years and had no idea I was being set up for a financial cliff. I called my insurer yesterday and found out they use an accumulator. I cried in the parking lot. But now I’m calling my doctor to ask about PAPs. I’m not alone. And I’m not giving up. 💪❤️
/p>Man, this hit hard. I’m from Ireland and we don’t have this mess-drugs are subsidized or free if you need them. But my sister lives in Texas and she’s on one of these cards. I showed her this post. She said, ‘I thought I was getting help.’ 😔
/p>Maybe we need to stop calling this ‘healthcare’ and start calling it what it is: a survival game with rigged rules.
Thanks for the clarity. 🙏
For anyone on a copay card: track your monthly usage religiously. Set a calendar reminder 30 days before your card’s annual limit is reached. Contact the manufacturer’s patient support line *before* you run out-they often have bridge programs or can fast-track you to a PAP. Don’t wait until your prescription is empty. Your body doesn’t pause for bureaucracy.
Also, ask your pharmacist for the name of your plan’s PBMs (pharmacy benefit manager). Call them directly. They’re the ones who decide whether to use accumulators or maximizers. Pharmacists don’t always know.
/p>okay but like… why does this even exist? who thought this was a good idea? ‘Let’s give people a temporary lifeline so they’ll keep paying for expensive drugs, then yank it away when they’re most vulnerable.’
/p>it’s not just cruel-it’s lazy. if the drug costs $2k a month, why isn’t the insurance company negotiating that? why isn’t the government stepping in? why are we all just… accepting this? i’m not mad, i’m just… disappointed. like, emotionally exhausted disappointed.
also-goodrx is a godsend. i use it for my anxiety med and it’s cheaper than my copay. i feel like a criminal for using it, but also… i’m not sorry.
My brother has diabetes. He uses GoodRx every month. Pays $25 for insulin. Insurance copay was $120. No card. No drama. Just cheaper. Simple.
Check prices. Always.
/p>Ever wonder why the cards have that tiny print saying ‘not valid for Medicare’? That’s not a legal footnote-it’s a warning. The system knows this is a trap. They want you on private insurance so they can use your copay money to inflate drug prices for everyone else. This is all connected. The same companies that make the drugs own the insurers. The same lobbyists who wrote this law sit in Congress. They’re not ‘helping.’ They’re harvesting. And you? You’re the crop.
They don’t want you to know this. That’s why this post is so rare. Don’t share it. Just use GoodRx. And pray.
/p>While the utility of manufacturer copay assistance cards is ostensibly beneficial, their structural integration into the commercial insurance ecosystem introduces significant moral hazard and perverse incentives. The absence of regulatory clarity regarding the inclusion of such payments in out-of-pocket maximum calculations constitutes a critical governance gap. One might reasonably posit that such mechanisms, while ostensibly altruistic, function as a form of market distortion that enables pharmaceutical entities to maintain artificially inflated pricing paradigms. The onus, therefore, must fall upon both regulatory bodies and policyholders to demand transparency and structural reform.
/p>