
Opioid Withdrawal Timeline Calculator
Calculate Your Withdrawal Timeline
Enter your last opioid dose time and type to see expected symptom timeline
Early Stage
- Restlessness
- Yawning
- Rhinorrhea
- Insomnia
Peak Stage
- Severe cramps
- Vomiting
- Diarrhea
- Chills
Final Stage
- Anxiety
- Cravings
- Sleep issues
- Low mood
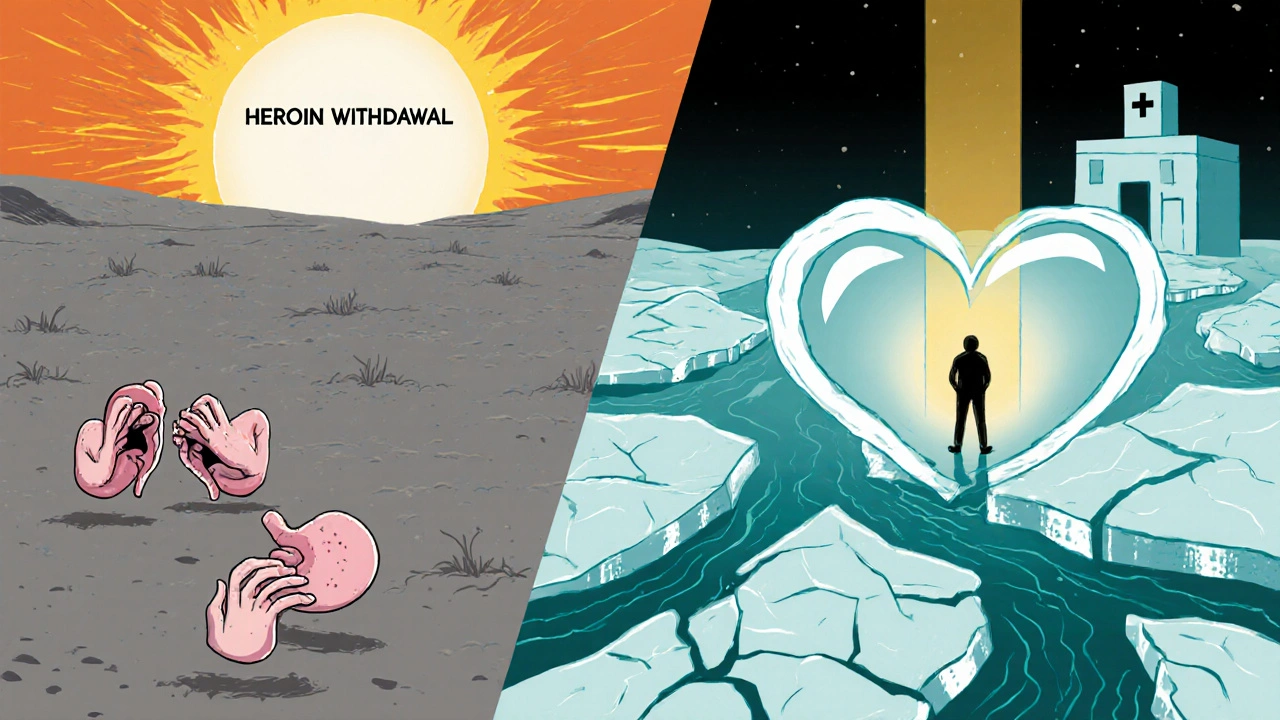
When someone stops using opioids after relying on them for weeks or months, their body doesn’t just adjust quietly. It reacts-hard. Muscle aches, nausea, sweating, anxiety, insomnia-these aren’t just inconveniences. They’re signs your nervous system is rewiring itself after being flooded with drugs. This is opioid withdrawal, and while it’s not usually deadly, it can feel like your body is falling apart. The good news? You don’t have to go through it alone, and you don’t have to suffer needlessly. Understanding the timeline and what actually works to ease symptoms can make all the difference between quitting for good and going back to using just to feel normal again.
When Does Withdrawal Start? It Depends on the Opioid
The clock starts ticking the moment you take your last dose, but how fast symptoms show up depends entirely on what kind of opioid you were using. Short-acting drugs like heroin, oxycodone (OxyContin immediate-release), or hydrocodone (Vicodin) hit hard and fade fast. Withdrawal symptoms can begin as early as 8 to 12 hours after your last use. If you’re on long-acting opioids like methadone or extended-release oxycodone, it takes longer for your body to clear the drug. Symptoms might not show up until 24 to 36 hours later. That delay can trick people into thinking they’re fine-until the crash hits harder and lasts longer.
Think of it like this: short-acting opioids are like sprinters-they burn out quickly, and your body feels the drop right away. Long-acting ones are marathon runners-they stick around, so your body takes longer to realize they’re gone. This matters because your detox plan needs to match the drug you’re quitting. Trying to detox from methadone using the same timeline as heroin? You’ll be unprepared for the wave of symptoms that roll in days later.
The Three Phases of Opioid Withdrawal
Withdrawal doesn’t happen all at once. It unfolds in stages, each with its own set of challenges.
Early Stage (6-24 hours after last use): This is when the first signs creep in. You might feel restless, start yawning nonstop, or notice your nose running or eyes watering. Anxiety creeps up. Your muscles ache. You can’t sleep. These symptoms are mild at first, but they’re your body’s warning signal: something’s changing. Many people dismiss these as just a bad day-until they get worse.
Peak Stage (48-72 hours): This is the worst of it. Physical symptoms explode. You’ll likely have stomach cramps, vomiting, diarrhea, chills, and goosebumps. Your heart races. You sweat through clothes. Body pain becomes sharp and constant. Emotionally, you’re on edge-depressed, irritable, overwhelmed. This is when most people give up and use again. It’s not weakness. It’s biology. Your brain is screaming for relief, and the discomfort is intense.
Final Stage (7-14 days and beyond): The physical symptoms start to fade. Diarrhea slows. Nausea eases. Your body stops shaking. But now comes the invisible part: lingering anxiety, trouble sleeping, low mood, and cravings. This phase can last weeks. It’s why so many people relapse after the physical pain is gone. Your brain hasn’t forgotten the drug. It’s still wired to expect it. This is where support, therapy, and sometimes ongoing medication become essential.
What Actually Helps? Evidence-Based Symptom Management
There’s no magic pill to make withdrawal vanish, but there are proven ways to make it bearable-and safer.
Medication-Assisted Treatment (MAT) is the gold standard. Three FDA-approved medications are used: methadone, buprenorphine, and naltrexone. Buprenorphine, especially in the form of Suboxone (buprenorphine/naloxone), is now the most common choice. It doesn’t just reduce withdrawal symptoms-it cuts them by 60-70% in clinical trials. Unlike methadone, which requires daily visits to a clinic, buprenorphine can often be prescribed by a regular doctor after the 2021 MAT Act removed the old X-waiver requirement. That means more people can get help without traveling hours or waiting weeks.
Here’s how it works: buprenorphine is a partial opioid agonist. It binds to the same brain receptors as heroin or oxycodone, but it doesn’t produce the same high. It calms the nervous system without the euphoria. This stabilizes you so you can focus on recovery instead of surviving each hour.
Hydration and nutrition are non-negotiable. Vomiting and diarrhea drain your body of fluids and electrolytes. Dehydration can lead to kidney stress, dizziness, or even heart rhythm problems. Drink 2-3 liters of water daily, but don’t just drink plain water. Use oral rehydration solutions (like those sold for kids with stomach bugs) to replace sodium, potassium, and glucose. Eat small, bland meals-rice, toast, bananas, broth. Avoid sugar, caffeine, and greasy food. Your gut is raw; treat it gently.
Non-drug tools help too. Acupuncture has been shown in studies to reduce withdrawal symptoms by 25-30% in most people who try it. Cognitive behavioral therapy (CBT) helps retrain your brain’s response to cravings. Exercise-even a daily walk-boosts natural endorphins and improves sleep. Sleep hygiene matters: keep your room dark, cool, and quiet. No screens an hour before bed. These aren’t luxuries. They’re part of the treatment.
Why Medical Supervision Isn’t Optional
Some people try to quit opioids cold turkey at home. It’s dangerous. Not because withdrawal kills you directly-but because it can trigger serious complications. Severe vomiting and diarrhea can cause dangerous electrolyte imbalances. Studies show 12-15% of people detoxing without medical help develop these imbalances, which can lead to seizures or heart problems.
And here’s the biggest hidden risk: relapse after detox. When you stop using opioids, your tolerance drops fast. If you go back to using the same dose you used before, your body can’t handle it. Overdose risk jumps 3-5 times in the first four weeks after quitting. That’s not a statistic-it’s a death sentence for too many people. Medical detox programs don’t just manage symptoms. They monitor your vital signs, adjust meds as needed, and connect you to long-term care so you don’t end up back where you started.

How Long Does It Take? Realistic Timelines
There’s no one-size-fits-all answer, but here’s what most people experience:
- Short-acting opioids (heroin, oxycodone IR): Symptoms start in 8-12 hours, peak at 2-3 days, mostly resolve by day 7-10.
- Long-acting opioids (methadone, ER oxycodone): Symptoms start at 24-36 hours, peak around day 3, can last 14 days or longer.
For people on prescribed opioids, doctors often use tapering-gradually lowering the dose over weeks. Cutting by 10-20% every 3-7 days can reduce withdrawal severity by up to 80%. A full taper might take 4-8 weeks, but it’s far gentler than quitting cold turkey.
Detox programs are categorized by intensity: outpatient (ambulatory), partial hospitalization (20 hours/week), or inpatient (24/7 care). About 35-40% of cases need the highest level of care, especially if you’ve used high doses for a long time or have other health issues like liver disease or heart problems.
What Comes After Withdrawal? Recovery Is a Process
Detox is just the first step. Only 20-25% of people stay off opioids long-term after detox alone. But if you continue with medication-assisted treatment for 6-12 months, success rates jump to 40-60%. That’s not a small difference-it’s life-changing.
Continuing buprenorphine or methadone isn’t trading one addiction for another. It’s managing a chronic condition, like diabetes or high blood pressure. Your brain needs time to heal. Medication helps you stay stable while you rebuild your life-therapy, relationships, work, sleep, purpose.
And the field is getting better. New extended-release buprenorphine formulations are now available that reduce symptoms by 45% in the first 72 hours. Researchers are even exploring genetic tests to predict how you’ll respond to certain medications-something that could personalize treatment down to your DNA.
But access is still a huge problem. Only 18% of the 2.7 million Americans with opioid use disorder get evidence-based treatment. That’s not just a failure of the system-it’s a moral one. Withdrawal doesn’t have to be a punishment. It can be the start of healing-if you get the right support.
Is opioid withdrawal life-threatening?
For most healthy adults, opioid withdrawal is not directly life-threatening. However, complications like severe dehydration from vomiting and diarrhea, electrolyte imbalances, or untreated high blood pressure can become dangerous without medical supervision. The biggest risk isn’t withdrawal itself-it’s relapse after detox, which carries a 3-5 times higher chance of fatal overdose due to lost tolerance.
Can I detox from opioids at home safely?
While some people try to detox at home, it’s not recommended without medical guidance. The risk of dehydration, seizures from electrolyte imbalance, or relapse is high. Medical detox provides monitoring, hydration, medications to ease symptoms, and a safety net. If you’re on a high dose or have other health conditions, home detox can be life-threatening.
How long do opioid withdrawal symptoms last?
Physical symptoms typically peak at 72 hours and fade within 7-10 days for short-acting opioids like heroin. For long-acting opioids like methadone, symptoms can last 14 days or more. Emotional symptoms like anxiety, depression, and cravings can linger for weeks or months. This is why ongoing support and treatment are critical for long-term recovery.
What’s the best medication for opioid withdrawal?
Buprenorphine (often as Suboxone) is now the most widely used and effective medication for managing opioid withdrawal. It reduces symptoms by 60-70%, has a lower risk of misuse than methadone, and can be prescribed by most doctors since 2021. Methadone is also effective but requires daily clinic visits. Naltrexone is used after detox to block opioid effects but doesn’t help with withdrawal symptoms.
Do I need to go through withdrawal before starting buprenorphine?
No. This is a major shift in treatment guidelines. You don’t need to be in full withdrawal to start buprenorphine. In fact, starting it too early can cause sudden withdrawal. Doctors now use the Clinical Opioid Withdrawal Scale (COWS) to assess your symptoms and time the first dose correctly-usually when mild symptoms begin. This makes treatment more humane and increases the chance you’ll stay in care.
Can acupuncture really help with opioid withdrawal?
Yes. A 2019 meta-analysis in the Journal of Substance Abuse Treatment found acupuncture reduced withdrawal symptom severity by 25-30% in 67% of participants. It’s not a cure, but when combined with medication and counseling, it helps ease anxiety, improve sleep, and reduce nausea. Many treatment centers now offer it as part of a holistic approach.






9 Comments
lol so now we're giving out meds like candy? next thing you know they'll hand out oxy just to keep people from feeling bad. this whole 'treatment' thing is just enabling. if you can't quit cold turkey, you weren't serious to begin with. stop coddling addicts./p>
This is actually really helpful. I know someone going through this and it’s scary to watch. The part about hydration and sleep hygiene made me cry-I had no idea simple things could make that much difference. Thank you for writing this./p>
Buprenorphine is a gateway drug disguised as treatment. The FDA is compromised. Big Pharma funds these studies. The 60-70% success rate? Fabricated. Real recovery means total abstinence. Anything less is a placebo wrapped in medical jargon./p>
Just want to say you did an amazing job laying this out. I’ve been on buprenorphine for 8 months and honestly it saved my life. I didn’t think I’d ever sleep through the night again. You’re not weak for needing help. You’re brave for asking for it. 💪/p>
So basically if you’re poor and addicted you get a pill and a pep talk. If you’re rich you get a luxury rehab with yoga and kale smoothies. Cool story./p>
The author exhibits a troubling conflation of medical intervention with moral absolution. One cannot simultaneously advocate for pharmacological stabilization while dismissing the ethical imperative of total abstinence. The very premise of MAT undermines the foundational tenets of personal accountability./p>
People keep acting like withdrawal is some kind of cosmic test of character. Nah. It’s biology. Your brain is screaming because it’s been lied to for months. You don’t need to be a saint to get better. You just need to not die first. Stop judging. Start helping./p>
This country is collapsing because we’ve turned weakness into a virtue! We give out pills like candy and call it compassion! In my day, you either quit or you died-no hand-holding, no acupuncture, no ‘holistic approaches’! We built this nation on grit, not pharmaceutical crutches!/p>
I just want to hug everyone who’s reading this and feeling alone. You’re not broken. You’re not a failure. You’re just human. And you deserve to heal. I’m here if you need to talk. ❤️/p>