Drug Side Effect Risk Assessment Tool
How this tool works
This tool helps you understand your personal risk of medication side effects based on key factors. It's not medical advice, but provides insights to help you have better conversations with your doctor.
Personalized Risk Assessment
Key recommendations for you:
When you take a medication, you expect it to help - not hurt. But side effects are part of the deal. Some are common, expected, and fade with time. Others come out of nowhere, even when you’ve done everything right. The difference between these two kinds of reactions isn’t just academic - it’s life-or-death. Understanding predictable vs unpredictable side effects helps you ask better questions, recognize danger early, and work smarter with your doctor.
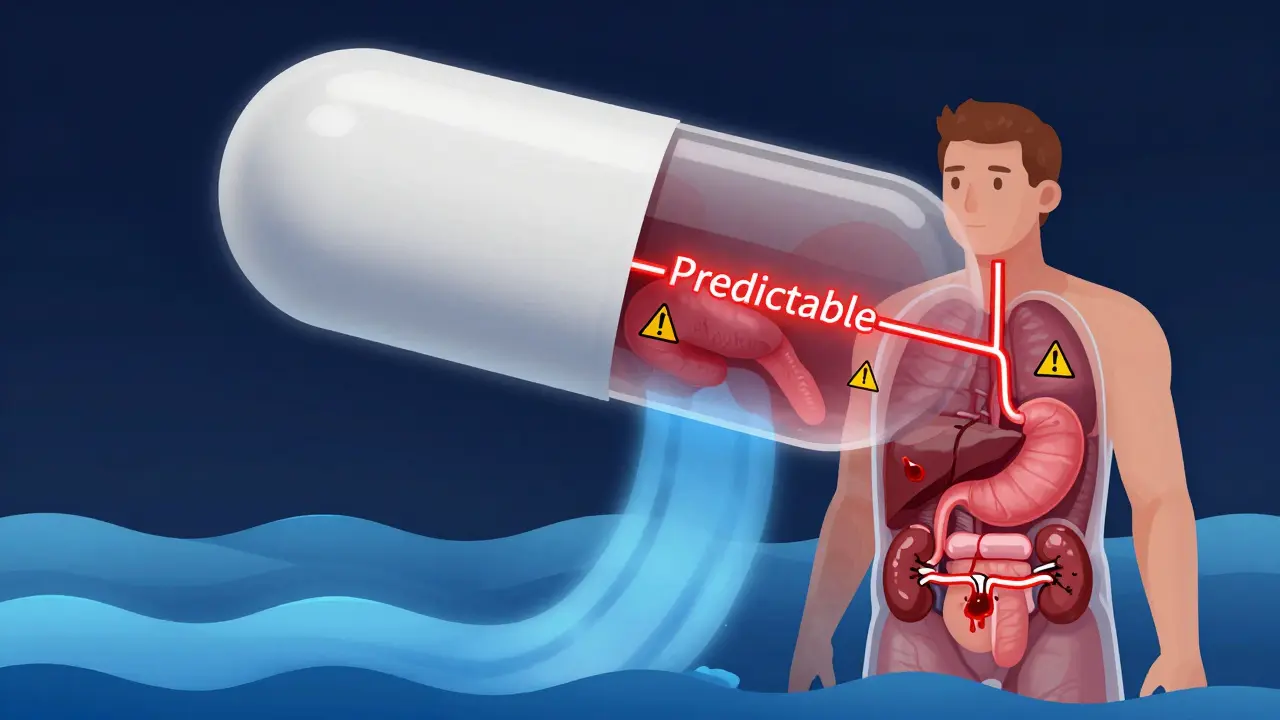
What Are Predictable Side Effects?
Predictable side effects, also called Type A reactions, make up 75 to 80% of all adverse drug reactions. They happen because the drug does exactly what it’s supposed to do - just too much, or in the wrong place. These aren’t mistakes. They’re extensions of the drug’s known action. Take NSAIDs like ibuprofen. They reduce inflammation and pain by blocking enzymes that make prostaglandins. But prostaglandins also protect your stomach lining. So when you take too much, or take it too long, you get stomach upset, ulcers, or even bleeding. That’s not random. It’s direct cause and effect. The higher the dose, the higher the risk. Studies show stomach bleeding jumps from 1-2% at normal doses to 10-15% at high doses. Other common predictable reactions:- Sedation from opioids or benzodiazepines
- Low blood pressure from blood pressure meds
- Low blood sugar from insulin or metformin
- Dry mouth from antihistamines
- Diarrhea from antibiotics
What Are Unpredictable Side Effects?
Unpredictable side effects, or Type B reactions, are the wild card. They happen in only 20-25% of cases, but they’re responsible for most serious injuries and drug withdrawals. There’s no warning. No clear dose pattern. No way to know who’s at risk - until it’s too late. These aren’t about how much you take. They’re about who you are. Your genes. Your immune system. Your body’s unique biology. Examples include:- Stevens-Johnson syndrome from carbamazepine or sulfonamides - a life-threatening skin reaction
- Anaphylaxis from penicillin - sudden swelling, trouble breathing, collapse
- Drug-induced hemolysis in people with G6PD deficiency - red blood cells break down after taking certain antibiotics or antimalarials
- Severe liver damage from acetaminophen in rare individuals - even at normal doses
Why the Difference Matters
The real value in knowing the difference isn’t just to label reactions - it’s to act on them. Predictable reactions? You can plan for them. Your doctor checks your kidney function before giving you NSAIDs. They monitor your blood sugar if you’re on metformin. They tell you to avoid alcohol with certain meds. These are standard precautions. You can reduce the risk. Unpredictable reactions? That’s where things get hard. There’s no test for most of them. No way to know if you’re at risk - unless you have a known genetic marker. For example, people of Han Chinese descent are often tested for HLA-B*1502 before taking carbamazepine. If they have it, they’re given a different drug. That single test prevents deadly skin reactions. But here’s the problem: we only have genetic tests for a few of these reactions. Right now, pharmacogenetic testing covers about 30% of high-risk Type B reactions. That means 70% still come out of nowhere. A 2020 case in The Lancet described a healthy 24-year-old who developed toxic epidermal necrolysis - a skin condition that kills 30% of those who get it - after taking a single dose of sulfamethoxazole. No prior allergies. No family history. No warning. Just a drug that turned deadly in one person out of 10,000.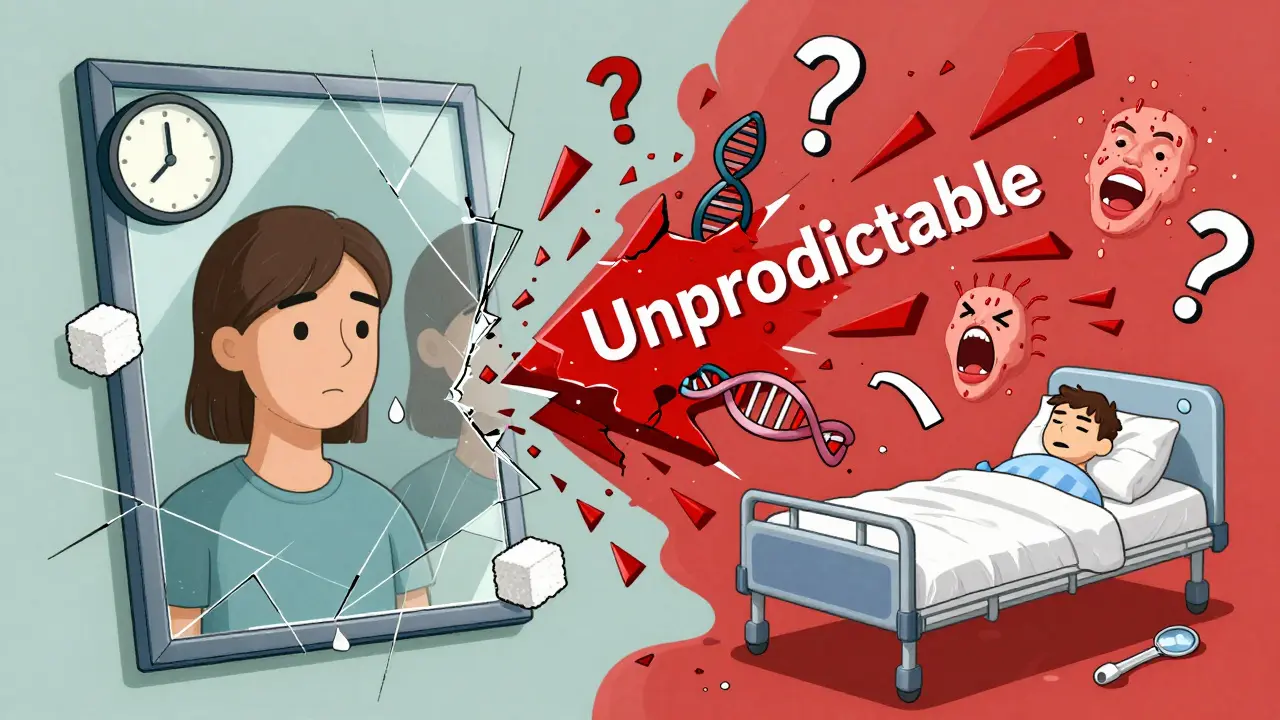
How Common Are They? The Numbers Don’t Lie
You might think unpredictable reactions are rare - and they are, in terms of frequency. But their impact is huge. - Type A reactions: 5 to 10 per 100 hospital admissions. Most are minor. Low death rate. - Type B reactions: 1 to 2 per 100 hospital admissions. But they cause 15 to 20% of all serious drug-related hospitalizations. Why? Because when a Type B reaction hits, it hits hard. Stevens-Johnson syndrome. Anaphylaxis. Liver failure. These aren’t side effects you can manage at home. They require ICU care, skin grafts, ventilators, or even organ transplants. The U.S. spends $30.1 billion a year treating adverse drug reactions. Of that, $22.6 billion goes to predictable reactions - because they happen so often. But $7.5 billion goes to unpredictable ones - because each one costs tens of thousands of dollars to treat.What Can You Do?
You can’t control your genes. But you can control your awareness. For predictable reactions:- Know your meds. Read the patient leaflet. Know the common side effects.
- Don’t ignore mild symptoms. Stomach pain after NSAIDs? Tell your doctor. It might be early warning.
- Ask if a lower dose or alternative drug is possible.
- Keep a symptom log. Note when side effects start and what you were taking.
- Know your family history. Has anyone had a severe reaction to a drug? Tell your doctor.
- Ask if genetic testing is available for your medication. Especially for drugs like abacavir (HIV), carbamazepine (seizures), or allopurinol (gout).
- Recognize red flags: rash, blistering, fever, swelling, trouble breathing, yellow skin, dark urine. These aren’t normal. Get help immediately.
- Carry a drug allergy card or use a medical ID app. If you’ve had one reaction, you’re at higher risk for others.

What’s Changing? The Future of Drug Safety
The field is moving fast. The FDA approved its first pharmacogenomic tool in 2023 to help doctors choose safer warfarin doses based on a patient’s genes. That’s a Type A win - reducing bleeding risk through precision. For Type B reactions, the NIH’s All of Us program has found 17 new gene-drug links - including ones that affect people outside the usual high-risk groups. That’s huge. It means we’re starting to see patterns we never noticed before. AI is helping too. Google Health trained a system on 10 million electronic health records. It predicted Type A reactions with 89% accuracy. But for Type B? Only 47%. That tells you everything you need to know: we’re good at spotting what’s expected. We’re still blind to what’s unexpected. The goal? Reduce severe unpredictable reactions by 50% by 2030. That’s ambitious. But possible - if we invest in genetic screening, better monitoring tools, and patient education.Final Thought: Safety Isn’t Just About the Drug
A drug isn’t safe or dangerous on its own. It’s safe or dangerous in you. Predictable side effects are the price of doing business. You can manage them. Unpredictable ones? They’re a lottery you didn’t sign up for. The more you know, the less you’re gambling. Talk to your pharmacist. Ask your doctor: "Is this drug known to cause rare but serious reactions? Should I be tested?" Don’t wait for a crisis to ask. Prevention starts with a conversation.Are all side effects dangerous?
No. Many side effects are mild and temporary - like drowsiness from antihistamines or nausea from antibiotics. These are usually predictable and not life-threatening. But any new or worsening symptom should be reported to your doctor. What seems minor today could be a sign of something more serious tomorrow.
Can I avoid unpredictable side effects entirely?
Not completely. Right now, we can only predict a small portion of them - mostly through genetic testing for specific drugs like abacavir or carbamazepine. For most others, there’s no test. The best you can do is know your family history, report any unusual reactions immediately, and avoid drugs you’ve reacted to before.
Do generics have the same side effects as brand-name drugs?
Yes. Generic drugs contain the same active ingredient as brand-name versions and are required to work the same way. That means they carry the same predictable and unpredictable side effects. Differences in inactive ingredients (like fillers or dyes) might cause rare allergic reactions in sensitive people, but the core drug effects are identical.
Why do some people react badly to a drug while others don’t?
It’s a mix of genetics, immune system differences, and sometimes unknown environmental factors. For example, the HLA-B*1502 gene variant makes some people extremely sensitive to carbamazepine. Others may have slower liver enzymes that cause drugs to build up. Some immune systems mistakenly attack drug-treated cells. We’re still learning why - but it’s never random. There’s always a biological reason, even if we haven’t found it yet.
Should I stop taking a drug if I get a side effect?
Never stop a prescribed medication without talking to your doctor first. Some side effects are normal and pass with time. Others need dose changes or added treatments. Stopping suddenly can be dangerous - especially with blood pressure meds, antidepressants, or seizure drugs. Always report the symptom, then let your doctor decide what to do next.
Are older adults more at risk for side effects?
Yes. As we age, our kidneys and liver process drugs more slowly. We often take multiple medications, increasing interaction risks. We’re also more likely to have chronic conditions that make side effects worse. About 25% of hospitalizations in seniors are due to adverse drug reactions - mostly predictable ones like bleeding, low blood sugar, or confusion from sedatives.
Can I trust online forums about drug side effects?
Online stories can raise awareness, but they’re not medical advice. Someone might say, “I got a rash from this drug,” but they might have had a virus at the same time. Or they took twice the dose. Always check with your doctor before making decisions based on forum posts. Reliable sources include the FDA, CDC, and your pharmacist.






10 Comments
Finally, someone breaks this down without fluff. Predictable side effects? Yeah, we know them. But the real danger is the ones that sneak up like a ghost-no warning, no pattern, just a single pill and your body turns on you. I’ve seen it. A friend took carbamazepine for migraines. One day, she had a rash. Next day, she was in the ICU. No prior history. No red flags. Just bad luck and a broken genetic lottery.
/p>Doctors act like they’ve got it all figured out. They don’t. We need mandatory pharmacogenomic screening for high-risk drugs-period. Not optional. Not ‘if you can afford it.’ This isn’t luxury medicine. It’s life-or-death triage.
And stop pretending generics are ‘the same.’ The active ingredient? Sure. But the fillers? The binders? Those can trigger Type B reactions in sensitive people. I’ve had patients react to the dye in a generic version of a drug they’d taken for years in brand form. It’s not placebo. It’s pharmacology.
We’re treating side effects like they’re glitches. They’re not. They’re biological signatures. We’re ignoring the data because it’s expensive. That’s not science. That’s negligence.
Oh honey, you’re telling me we’re still playing Russian roulette with prescriptions? 😅
/p>Let me get this straight-your doctor gives you a pill, and you’re supposed to just ‘hope’ you don’t become a human cautionary tale? Meanwhile, the FDA approves new drugs faster than my ex texts me after midnight.
I had my aunt go into liver failure from acetaminophen. Normal dose. No alcohol. No overdose. Just… her liver said ‘nope.’ No test. No warning. Just a $2 bottle of Tylenol and a $500k ICU bill.
And now you want me to ‘talk to my pharmacist’? Sweetie, my pharmacist doesn’t know what’s in my DNA. He just knows I’m buying cough syrup again.
Stop treating patients like lab rats and start testing like we’re trying to save lives. Not just hit quarterly profit targets.
Also-why is this still a ‘discussion’ in 2025? 🤡
It’s so frustrating to see people treat drug safety like a buffet. ‘Oh, I’ll just take a little extra because I feel like it.’ No. You’re not a chef. You’re a patient. And patients who ignore predictable side effects? They’re the reason we have so many preventable ER visits.
/p>And don’t even get me started on the ‘I read it on Reddit’ crowd. You think your cousin’s friend’s dog had a reaction to penicillin means you’re allergic? Please. You’re not a doctor. You’re a data point with a smartphone.
Genetic testing? Yes. But only for those with family history. Not everyone needs it. We’re not all genetically doomed. Some of us have normal immune systems.
And before you say ‘it’s a human right’-no, it’s not. It’s medicine. And medicine requires responsibility. Not panic. Not fearmongering. Just… common sense.
I appreciate this breakdown. I’ve been on metformin for 8 years and never had a problem-until last month, I started feeling dizzy after meals. I didn’t think much of it until I checked my blood sugar and it was 52. I called my doctor. We lowered the dose. Simple fix.
/p>That’s the thing-predictable doesn’t mean harmless. It means *knowable*. And knowing is power.
But the unpredictable ones… they haunt me. My neighbor’s son took allopurinol for gout. One rash. One hospital stay. Now he’s on dialysis. No family history. No prior issues. Just… biology being cruel.
I’ve started asking my doctor: ‘Is there a genetic test for this?’ He laughs. Says it’s ‘not cost-effective.’ I say: ‘What’s the cost of a kidney?’
We need to stop treating prevention like an expense. It’s an investment.
And yes-I carry a medical ID card now. Because I don’t want to be the next ‘one in 10,000’ story.
Y’all are overthinking this. I’ve been on 12 different meds in 5 years. Got stomach cramps, drowsiness, dry mouth-whatever. I just deal. If I feel weird, I stop. Done.
/p>My grandma lived to 98. Never saw a doctor. Took aspirin every day. Never had a problem.
Stop scaring people. It’s just pills. You’re not a lab mouse. Chill.
For those worried about unpredictable reactions: you’re not powerless. You can still take control.
/p>1. Keep a written log of every medication you take-name, dose, date, symptoms. Even if it’s ‘just a headache.’
2. Tell every new provider about every past reaction-even if it was ‘mild.’
3. Ask: ‘Has this drug been linked to any rare reactions in people my age, gender, or ethnicity?’
4. Use apps like Medisafe or MyTherapy to track and share with your doctor.
And if you’ve ever had a rash, swelling, or fever after a new drug? Flag it. Don’t wait. That’s your body screaming.
Most Type B reactions aren’t random. They’re unreported. We’re missing the pattern because we’re not listening.
Be your own advocate. Not because you distrust doctors. But because you care enough to show up.
Let’s be honest: the real issue isn’t drug safety-it’s American healthcare’s obsession with profit over prevention. We don’t test for genetic risks because it cuts into Big Pharma’s margins. We don’t mandate screening because it’s ‘too expensive.’
/p>Meanwhile, the U.S. spends more per capita on healthcare than any nation on Earth-and still has the highest rate of preventable drug injuries.
And yet, we still act like we’re the global leader in medical innovation? Please. We’re the land of ‘fix it after it breaks.’
It’s not the drugs. It’s the system. And until we fix that, no amount of ‘patient education’ will save you.
Given the current pharmacovigilance paradigm, the dichotomy between Type A and Type B adverse drug reactions (ADRs) remains a critical axis for risk stratification. Type A reactions, being pharmacologically predictable, are amenable to dose-response modeling and pharmacokinetic optimization, as evidenced by the 75–80% prevalence in clinical cohorts.
/p>Conversely, Type B reactions, which are idiosyncratic and immunologically mediated, present a significant challenge to predictive modeling due to their low incidence and heterogeneous etiology. Recent studies utilizing genome-wide association studies (GWAS) have identified HLA alleles as primary risk determinants for hypersensitivity syndromes such as Stevens-Johnson syndrome (SJS) and drug reaction with eosinophilia and systemic symptoms (DRESS).
However, the current clinical implementation of pharmacogenomic screening remains suboptimal. The FDA’s 2023 approval of warfarin pharmacogenomic guidance represents a milestone, yet coverage for high-risk agents such as carbamazepine, abacavir, and allopurinol remains inconsistent across payers.
Furthermore, the absence of validated biomarkers for non-HLA-mediated Type B reactions-such as acetaminophen-induced hepatotoxicity in non-alcoholic individuals-underscores the necessity for longitudinal biobanking and AI-driven phenotyping. The NIH’s All of Us initiative, while promising, requires accelerated data integration into EHR systems to enable real-time clinical decision support.
Until we institutionalize preemptive genotyping as standard of care for high-risk medications, Type B reactions will remain an unacceptable burden on healthcare systems and patients alike.
Wow. A 2000-word essay on why drugs are dangerous. Congrats. You just made me want to never take another pill.
/p>So… what’s the solution? Stop taking medicine? That’s not a plan. That’s a panic attack.
Also, ‘genetic testing’? Cool. How much does that cost? $500? $2000? Who’s paying? My insurance? The hospital? You?
And let’s be real-most people don’t even know what their blood type is. You think they’re gonna get a DNA test before taking ibuprofen?
Stop overcomplicating it. If you feel weird, call your doctor. If you’re scared, don’t take it. Simple. Not sexy. But it works.
As someone from India, I’ve seen this play out differently.
/p>Here, people often take antibiotics without prescriptions. They finish half the course. Then they get sick again. Then they take more. It’s not about unpredictable reactions-it’s about misuse.
But when it comes to Type B reactions? We’re even less prepared. Genetic testing? Almost non-existent in rural clinics.
What we need isn’t just better science-it’s better access. A woman in Bihar shouldn’t have to die because her doctor never heard of HLA-B*1502.
Maybe the answer isn’t just testing everyone in the U.S.-but teaching every doctor, everywhere, to ask: ‘Has anyone in your family ever had a bad reaction to medicine?’
Simple questions. Life-saving answers.
And yes-I’ve had a rash from a painkiller too. I told my doctor. He switched it. No big deal. But I didn’t ignore it.
That’s the real lesson: listen to your body. Even if the system doesn’t listen to you.