Liver function: read your tests and protect your liver
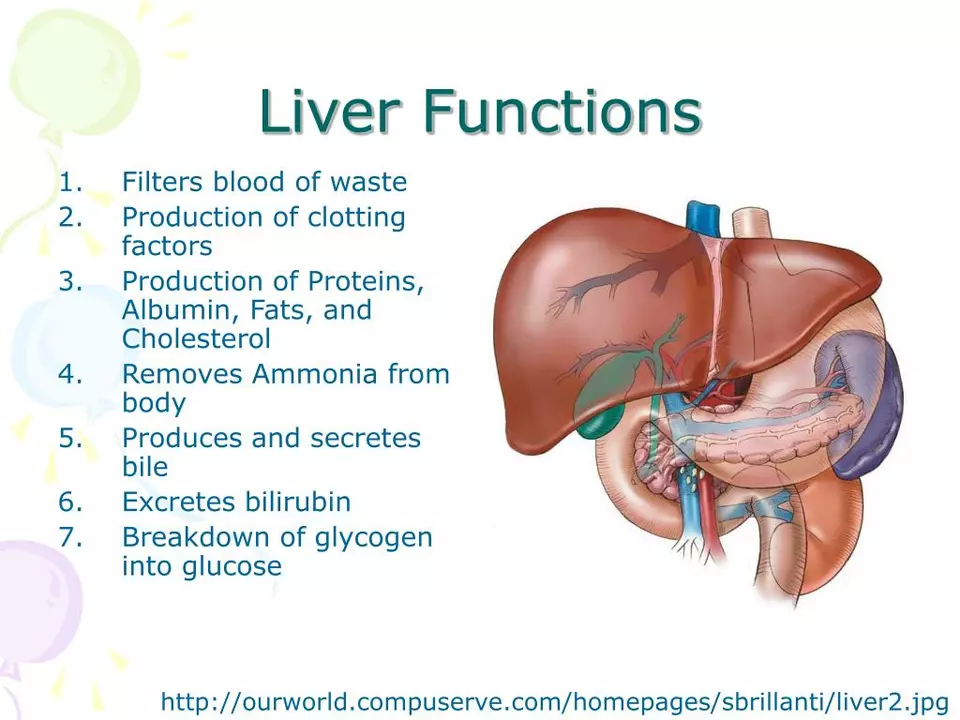
Want a simple way to understand liver function? Your liver does dozens of jobs: filters toxins, stores energy, and makes proteins your body needs. When it struggles, tests and a few smart habits tell you early so you can act fast.
What the common tests mean
Doctors usually order LFTs — that means ALT, AST, ALP, GGT, bilirubin, albumin and sometimes INR. ALT and AST rise when liver cells are damaged. High ALP or GGT can point to blocked bile flow. Bilirubin makes your skin or eyes look yellow when it’s high. Low albumin or a prolonged INR shows your liver’s ability to make important proteins is falling. One high number doesn’t always mean severe disease, but repeating tests and comparing trends matters.
Want specifics? If ALT or AST are mildly raised (under about two or three times normal), we often watch and repeat the test. Big jumps or symptoms like jaundice, belly pain, or confusion need urgent checks.
Medications, supplements and things that hurt the liver
Some common drugs can raise liver enzymes or cause injury. Acetaminophen at high doses is a top cause — don’t exceed the daily limit on the bottle and check with your doctor if you drink alcohol. Statins and proteins in combination meds (like Vytorin) can raise enzymes for some people; doctors usually check LFTs before and a few months after starting them. Other culprits: methotrexate, isoniazid, valproate, some antibiotics (for example amoxicillin–clavulanate), and certain herbal products like kava or high-dose green tea extracts.
Always tell your clinician about over-the-counter meds and supplements. If a drug is necessary, your doctor may monitor LFTs on a schedule — often baseline, then 6–12 weeks after start, then less often if stable.
How do you spot trouble early? Watch for dark urine, pale stools, yellowing of eyes, itchy skin, unusual tiredness, persistent nausea, belly pain or easy bruising. Any of these deserve a call to your provider.
Easy ways to protect your liver: avoid heavy alcohol, follow medication doses, get vaccinated for hepatitis A and B if you’re at risk, use condoms or avoid sharing needles, and keep a healthy weight to reduce fatty liver. If you have chronic viral hepatitis, new treatments can cure hepatitis C and control hepatitis B — ask your doctor.
If tests look off, expect repeat bloodwork, possible abdominal ultrasound or a FibroScan to check scarring, and sometimes referral to a liver specialist. Don’t ignore small changes — early action usually prevents bigger problems.
Questions about a specific drug or test result? Bring the pill bottle and lab printout to your next visit. That makes it quicker to spot risks and plan the right follow-up.
Teriflunomide and Liver Function: Monitoring and Managing Risks
In today's blog post, we'll be discussing Teriflunomide and its effects on liver function. Teriflunomide is a drug used to treat multiple sclerosis, but it comes with some potential risks to our liver. It's essential to closely monitor liver function while taking this medication to manage and mitigate any possible side effects. We'll delve into the importance of regular liver function tests and explore some tips on maintaining a healthy liver while using Teriflunomide. Stay tuned for practical advice on ensuring your liver stays in top shape while benefiting from this treatment.