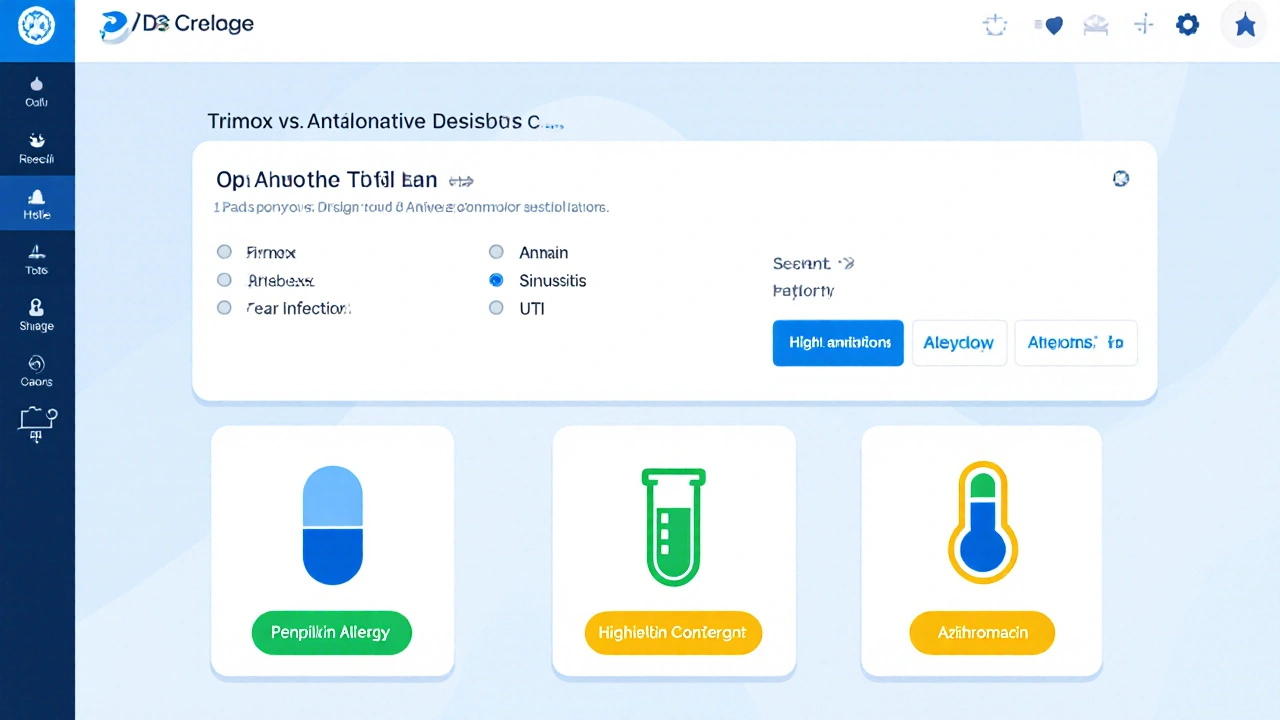
Trimox vs Alternative Antibiotics Decision Guide
Enter your infection type and patient profile, then click Compare to see which antibiotic may be best for you.
Trimox (Amoxicillin)
Broad-spectrum penicillin, cost-effective, first-line for common infections.
Augmentin
Amoxicillin + clavulanic acid, broader coverage against resistant bacteria.
Azithromycin
Macrolide with convenient once-daily dosing, good for respiratory infections.
When a doctor writes a prescription for a common infection, the name on the label can feel like a code you need to crack. One of the most frequently seen names is Trimox is a branded form of the antibiotic amoxicillin, used to treat a wide range of bacterial infections. But does Trimox always make the best choice? How does it stack up against other antibiotics you might hear about, like Augmentin or azithromycin? This guide breaks down the facts, side‑by‑side, so you can see when Trimox shines and when another option might be safer or more effective.
Key Takeaways
- Trimox (amoxicillin) is a broad‑spectrum penicillin‑type antibiotic, ideal for many mild‑to‑moderate infections.
- Alternatives such as Augmentin, doxycycline, and azithromycin cover some bacteria that amoxicillin can’t, but they often come with higher cost or more side‑effects.
- Choosing the right antibiotic depends on infection type, patient allergies, local resistance patterns, and dosing convenience.
- All antibiotics carry a risk of resistance; completing the full course is critical regardless of the drug.
- Consult a pharmacist or prescriber if you’re unsure which option fits your health situation.
What Is Trimox (Amoxicillin)?
Amoxicillin is a beta‑lactam antibiotic belonging to the penicillin class, effective against many Gram‑positive and some Gram‑negative bacteria. It works by inhibiting the bacterial cell wall synthesis, which leads to cell lysis and death. In Australia, the standard adult dose for most infections is 500mg three times daily, though pediatric dosing is weight‑based (usually 20‑40mg/kg/day divided into two or three doses).
Common conditions treated with Trimox include ear infections (otitis media), sinusitis, uncomplicated urinary tract infections, and certain skin infections. Because it’s generally well tolerated, Trimox is often the first‑line choice for doctors who want a single‑pill regimen without a beta‑lactamase inhibitor.
How Amoxicillin Works and Its Limitations
The drug targets the transpeptidase enzymes that cross‑link peptidoglycan strands in bacterial cell walls. By binding irreversibly to these enzymes, amoxicillin prevents the wall from strengthening, causing the bacteria to burst under osmotic pressure.
However, many bacteria produce beta‑lactamase enzymes that break down amoxicillin before it can act. In such cases, a beta‑lactamase inhibitor (like clavulanic acid) is added, creating a combo drug such as Augmentin. Also, amoxicillin has limited activity against certain atypical pathogens (e.g., Mycoplasma, Chlamydia) and some resistant strains of Streptococcus pneumoniae.
When Doctors Prescribe Trimox
Clinicians follow local guidelines-like the Australian Therapeutic Guidelines-for selecting antibiotics. Trimox is typically recommended when:
- The suspected pathogen is known to be sensitive to penicillins.
- The patient has no documented penicillin allergy.
- The infection is uncomplicated and not caused by beta‑lactamase‑producing bacteria.
- The cost and dosing frequency need to be low for better adherence.
If any of these conditions aren’t met, the prescriber may jump to an alternative.
Overview of Common Alternatives
Below are the most frequently considered substitutes when amoxicillin isn’t ideal.
- Augmentin (amoxicillin/clavulanic acid) - adds a beta‑lactamase inhibitor to broaden coverage.
- Doxycycline - a tetracycline that works well for atypical organisms and some resistant strains.
- Azithromycin - a macrolide with once‑daily dosing, useful for respiratory tract infections.
- Cefalexin - a first‑generation cephalosporin, often chosen for skin infections when penicillin allergy exists.
- Clarithromycin - another macrolide, stronger against certain resistant strains of Streptococcus pneumoniae.
Side‑By‑Side Comparison Table
| Antibiotic | Class | Typical Dose (Adult) | Coverage Strength | Common Side‑effects | Cost (AU$) per Course* |
|---|---|---|---|---|---|
| Trimox (Amoxicillin) | Penicillin | 500mg TID for 7‑10 days | Broad Gram‑positive, limited Gram‑negative | GI upset, rash, rare liver issues | ≈8-12 |
| Augmentin (Amox/Clav) | Penicillin + β‑lactamase inhibitor | 875mg/125mg BID for 7‑10 days | Broad Gram‑positive, many β‑lactamase producers | Diarrhea, metallic taste, liver enzyme rise | ≈15-22 |
| Doxycycline | Tetracycline | 100mg BID for 7‑14 days | Atypical pathogens, some resistant Gram‑negatives | Photosensitivity, esophageal irritation | ≈12-18 |
| Azithromycin | Macrolide | 500mg day1 then 250mg daily x4 days | Respiratory, some STIs, limited Gram‑negatives | GI upset, QT prolongation (rare) | ≈20-28 |
| Cefalexin | Cephalosporin (1st gen) | 500mg QID for 7‑10 days | Skin, bone, urinary isolates; pen‑allergy safe | Diarrhea, rash, mild liver effects | ≈14-20 |
*Prices are approximate retail costs in Australian pharmacies (2025). Exact figures vary by pharmacy and insurance coverage.
Decision Factors: When to Choose Trimox vs an Alternative
Picking the right antibiotic is a balancing act. Consider these practical checkpoints:
- Pathogen suspicion: If you suspect a beta‑lactamase‑producing organism (e.g., Haemophilus influenzae), Augmentin often outperforms plain amoxicillin.
- Allergy profile: Anyone with a documented penicillin allergy should avoid Trimox and consider cefalexin or a macrolide.
- Convenience: Azithromycin’s short 5‑day course can improve adherence for busy patients.
- Cost constraints: Trimox remains the cheapest broad‑spectrum option, a key factor for uninsured patients.
- Resistance trends: Local antibiograms-public health reports on bacterial susceptibility-may show rising amoxicillin resistance for certain community‑acquired pneumonia, nudging prescribers toward doxycycline or a macrolide.
When two drugs appear equally viable, the simpler dosing schedule (once or twice daily) usually wins because patients are less likely to miss a dose.
Safety, Interactions, and Resistance
All antibiotics disrupt normal gut flora, which can lead to Clostridioides difficile infection in rare cases. The risk is slightly higher with broad‑spectrum agents like Augmentin.
Key drug interactions to watch for:
- Trimox: May reduce the effectiveness of oral contraceptives-use backup contraception.
- Azithromycin: Interacts with drugs that affect heart rhythm (e.g., certain antiarrhythmics).
- Doxycycline: Calcium‑rich foods or antacids can lower absorption; take on an empty stomach.
Regardless of the choice, completing the full prescribed course is essential. Stopping early can leave surviving bacteria, fostering resistance that makes future infections harder to treat.
How to Talk to Your Pharmacist or Doctor
If you receive a prescription and aren’t sure why that specific antibiotic was chosen, bring these questions:
- What infection is being treated and which bacteria are most likely?
- Do I have any allergies that would make this drug unsafe?
- Is there a cheaper or simpler alternative that would work just as well?
- What side‑effects should I watch for, and when should I seek medical help?
A clear conversation can prevent unnecessary exposure to broad‑spectrum agents and keep resistance rates down.
Quick FAQ
Frequently Asked Questions
Can I use Trimox for a sore throat?
If the sore throat is caused by a bacterial infection like streptococcal pharyngitis, Trimox is an appropriate first‑line choice, provided you’re not allergic to penicillins.
What should I do if I miss a dose of Trimox?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one-don’t double‑dose.
Is Augmentin stronger than Trimox?
Augmentin adds clavulanic acid, which blocks beta‑lactamase enzymes. This makes it effective against bacteria that would otherwise destroy plain amoxicillin, so in that sense it’s broader and often considered “stronger.”
Can I take Trimox and a probiotic together?
Yes. Taking a probiotic a few hours after the antibiotic can help restore gut flora, though it won’t interfere with Trimox’s effectiveness.
Why do some doctors prescribe a 5‑day azithromycin instead of a 10‑day amoxicillin?
Azithromycin’s long half‑life allows a short, once‑daily regimen, which can improve adherence, especially for respiratory infections where the likely pathogens are macrolide‑sensitive.
In a nutshell, Trimox remains a solid, cost‑effective option for many routine infections, but the landscape of bacterial resistance and patient‑specific factors means alternatives like Augmentin, doxycycline, or azithromycin can be better fits in certain scenarios. Always let the prescriber know your medical history, and don’t hesitate to ask a pharmacist to clarify why a particular drug was chosen for you.






15 Comments
Trimox remains a first‑line option because it covers the majority of community‑acquired pathogens while maintaining a low adverse‑event profile and cost.
/p>Look, I get it – you read the article and think amoxicillin is just a magic bullet, but the reality is far messier than that. The rise of beta‑lactamase‑producing H. influenzae has turned many simple ear‑infections into a therapeutic nightmare. Augmentin may cost more, but it’s literally saving lives where plain Trimox would be ripped apart by those enzymes.
/p>And don’t even get me started on the macrolide resistance in Streptococcus pneumoniae – azithromycin is not a free‑for‑all option any more, it’s a gamble you shouldn’t make unless you have a crystal‑clear indication.
The pharmacoeconomic argument for Trimox holds only when you’re dealing with a susceptible strain, not when local antibiograms scream “high resistance”.
Patients with a penicillin allergy aren’t just “somewhat allergic”; cross‑reactivity can be life‑threatening, so swapping to cefalexin or a macrolide is not a matter of preference, it’s a safety imperative.
And the notion that “shorter courses are always better” is a myth – you still need an adequate duration to prevent relapse and eventual resistance selection, especially in UTIs.
Side‑effects? Sure, everyone gets GI upset, but the risk of C. difficile colitis rises dramatically with broad‑spectrum agents like Augmentin.
Drug interactions matter too – remember that azithromycin can prolong the QT interval, a big red flag for those on antiarrhythmics.
Bottom line: the decision tree in the guide is helpful, but you need to overlay it with local resistance data and individual patient factors – otherwise you’re just guessing.
And yes, completing the full course is non‑negotiable; stopping early is the fastest way to nurture super‑bugs.
Finally, cost isn’t just about the price tag of the pill – think about downstream expenses from treatment failures and hospitalizations.
So before you claim Trimox is always the cheapest, ask yourself what the hidden costs might be.
In short, use Trimox when it truly fits, but don’t be afraid to pivot to a broader agent when the clinical picture calls for it.
Oh great, another “one‑size‑fits‑all” antibiotic suggestion – how original.
/p>Hey, let’s not discount Trimox just because there are alternatives – it’s like saying every curry needs extra chili. In many settings, especially where the local bacteria haven’t developed heavy resistance, amoxicillin still does the job beautifully. Plus, the dosing schedule is friendly: three times a day, not the hassle of a twice‑daily high‑dose Augmentin.
/p>And you know what? The color‑ful world of antibiotics isn’t just about “stronger” – it’s about matching the right weapon to the right battle. Sometimes a simple sword cuts cleaner than a fancy, over‑engineered bazooka.
👍 Trimox is cheap and works for many infections, but always check your local resistance patterns! 🌍
/p>While the guide paints a tidy picture, one must remember that the pharmaceutical market thrives on nuance. The assumption that cost alone dictates the best choice ignores the hidden expenses of treatment failures. For instance, prescribing Trimox in a region where beta‑lactamase prevalence exceeds 30 % may result in a higher rate of therapeutic failure, ultimately costing insurers and patients more due to subsequent visits, lab work, and alternative prescriptions. Moreover, the psychological impact of persistent infection cannot be dismissed; patient confidence wanes when initial therapy falters, potentially leading to non‑adherence in future regimens.
/p>One should also consider the ecological impact: broader‑spectrum agents like Augmentin exert greater selective pressure on the microbiome, fostering resistant flora. From a stewardship perspective, reserving such agents for proven indications aligns with best practices.
Therefore, the decision matrix should be weighted not merely by price and convenience but by a composite of local antibiograms, patient comorbidities, and the anticipated burden of resistance. Only then can we claim a truly evidence‑based approach.
Trimox is often enough for a simple sore throat 😊.
/p>Consider the philosophical undertones of antibiotic selection: each dose is a pact with the unseen microbial world, a delicate balance between eradication and coexistence. When we default to the most potent agent, we risk upsetting that equilibrium, inviting the rise of super‑bugs. Yet, when we under‑treat, we betray our patients’ trust. The moral imperative, therefore, is to align clinical judgement with humility, acknowledging that our prescriptions echo far beyond the immediate infection.
/p>Trimox is cheap and works for many infections but not for those with beta‑lactamase producing bacteria
/p>From a clinical informatics standpoint, the decision algorithm should integrate real‑time antibiogram data, pharmacokinetic modeling, and patient‑specific variables like renal function to dynamically recommend the optimal agent, rather than relying on static tables.
/p>Good rundown! Just remember to ask your doctor about any allergies and check if your insurance covers the chosen antibiotic.
/p>Insurance coverage is a nightmare, especially when the pharmacy pushes the pricey combo when a cheap generic would do. Fight the system, demand a prescription audit!
/p>Honestly, the guide is just a marketing fluff piece – pick what's actually prescribed in your clinic.
/p>Totally get that frustration, but keeping an open mind helps find the right fit for each patient.
/p>Nice info thanks for sharing
/p>