When doctors prescribe opioids for severe pain-after surgery, cancer treatment, or a major injury-they’re not just giving you relief. They’re also giving you a set of predictable, often stubborn side effects. For many people, constipation, drowsiness, and nausea become part of daily life while taking these medications. Unlike a headache or a rash, these aren’t temporary annoyances. They stick around. And if you don’t plan for them, they can make life harder than the pain you’re trying to treat.
Constipation: The Most Common, and Most Overlooked, Side Effect
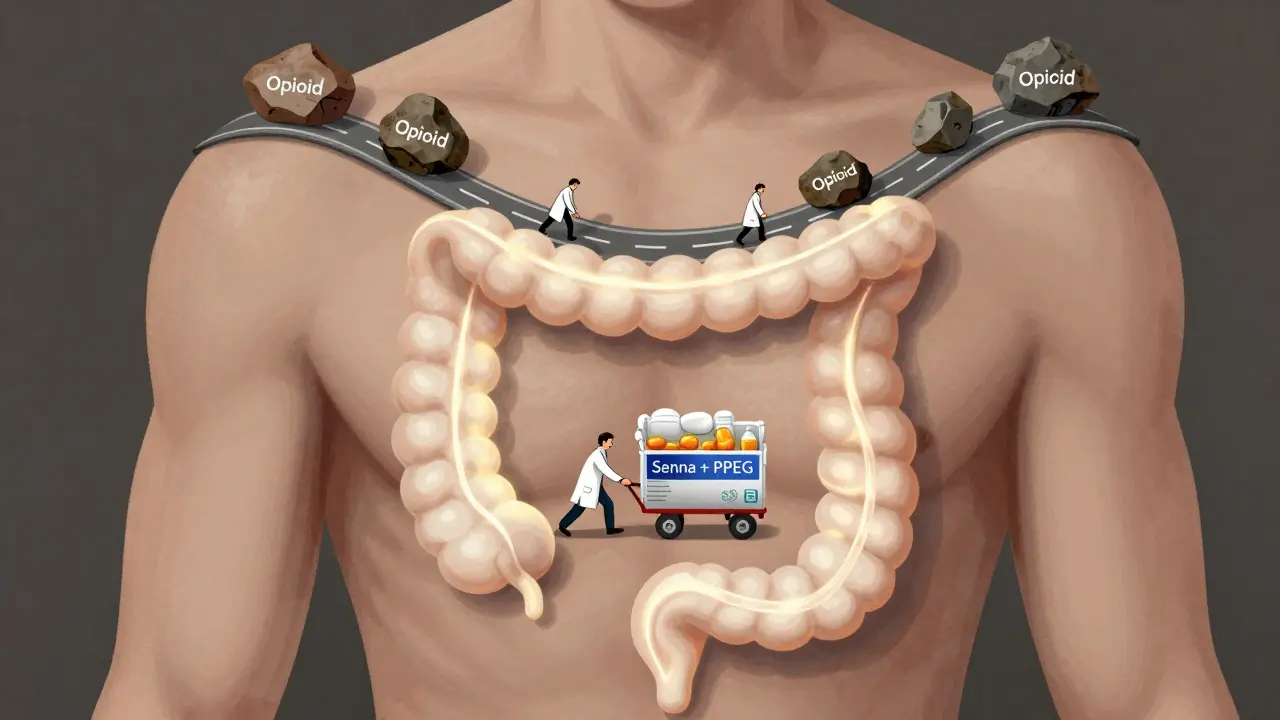
If you’re on opioids long-term, constipation isn’t a possibility-it’s a guarantee. Studies show nearly every patient who takes opioids for more than a few weeks will experience it. Why? Because opioids don’t just block pain signals in your brain. They also latch onto receptors in your gut, slowing down the natural muscle contractions that move food through your intestines. The result? Stools become hard, dry, and painfully difficult to pass. Unlike drowsiness or nausea, which often fade after a week or two, constipation doesn’t improve with time. Your body doesn’t build tolerance to it. That’s why experts say you shouldn’t wait until you’re struggling to go. Start treatment for constipation the same day you start opioids. Prophylactic laxatives aren’t optional-they’re essential. The most effective approach combines two types of laxatives: a stimulant like senna to get things moving, and an osmotic agent like polyethylene glycol to pull water into the colon. Drink plenty of fluids. Eat fiber-rich foods. Stay active. These help, but they’re rarely enough on their own. If over-the-counter options fail, medications like methylnaltrexone (Relistor) or naloxegol (Movantik) are designed specifically for opioid-induced constipation. They work in the gut without touching the pain-relieving effects in your brain. Ignoring constipation doesn’t just make you uncomfortable. It can lead to bowel obstruction, hemorrhoids, or even hospitalization. Don’t wait until it’s severe. Talk to your doctor before your first dose.Drowsiness: When Your Brain Feels Like It’s Wading Through Mud
You take your opioid, and suddenly everything feels slower. Your thoughts are foggy. Your eyelids are heavy. You feel like you’ve been up for three days-even if you slept eight hours. That’s not laziness. That’s the drug working exactly as it’s supposed to. Opioids depress the central nervous system. That’s how they reduce pain. But it also reduces alertness. Between 20% and 60% of people starting opioids report drowsiness. For most, it fades after a few days as the body adjusts. But for about 1 in 10 long-term users, the fog never lifts. That’s a problem if you drive, work with machinery, or care for children. Even mild drowsiness increases the risk of falls and accidents. The key is timing. Take your dose at night if possible. Avoid alcohol, benzodiazepines like Xanax, or sleep aids-they multiply the sedation and can be deadly. If drowsiness persists beyond two weeks, don’t just push through it. Talk to your doctor. A small dose reduction might help. In rare cases, stimulants like methylphenidate (Ritalin) are used off-label, but there’s little solid evidence they work consistently, and they come with their own risks. Also, review all your other medications. Some antidepressants, antihistamines, and muscle relaxants make drowsiness worse. Eliminating unnecessary drugs can make a big difference.Nausea: Why Your Stomach Feels Like It’s in Revolt
Nausea hits about one in four people when they start opioids. It’s not just feeling queasy-it’s the urge to vomit, often without warning. The reason? Opioids trigger a part of your brain called the chemoreceptor trigger zone. They also slow down your stomach emptying, which makes food sit and ferment, adding to the discomfort. The good news? For most people, nausea fades within 3 to 7 days. Your body adapts. But for 1 in 10 long-term users, it doesn’t. And when nausea sticks around, it makes people skip doses-or stop the medication entirely. That means uncontrolled pain. That’s the opposite of what you want. Treatment starts with anti-nausea meds. The most common first choice is metoclopramide or prochlorperazine-drugs that block dopamine, one of the main triggers. If those don’t work, ondansetron (Zofran), which targets serotonin, can help. Promethazine (Phenergan) is another option, especially if you’re also having trouble sleeping. Don’t try to tough it out. If nausea lasts more than a week, ask for help. Your doctor can switch you to a different opioid. Some, like tramadol or buprenorphine, are less likely to cause nausea. Or they can adjust your dose. Starting low and going slow-taking a smaller dose at first and increasing it gradually-is the best way to avoid severe nausea from the start.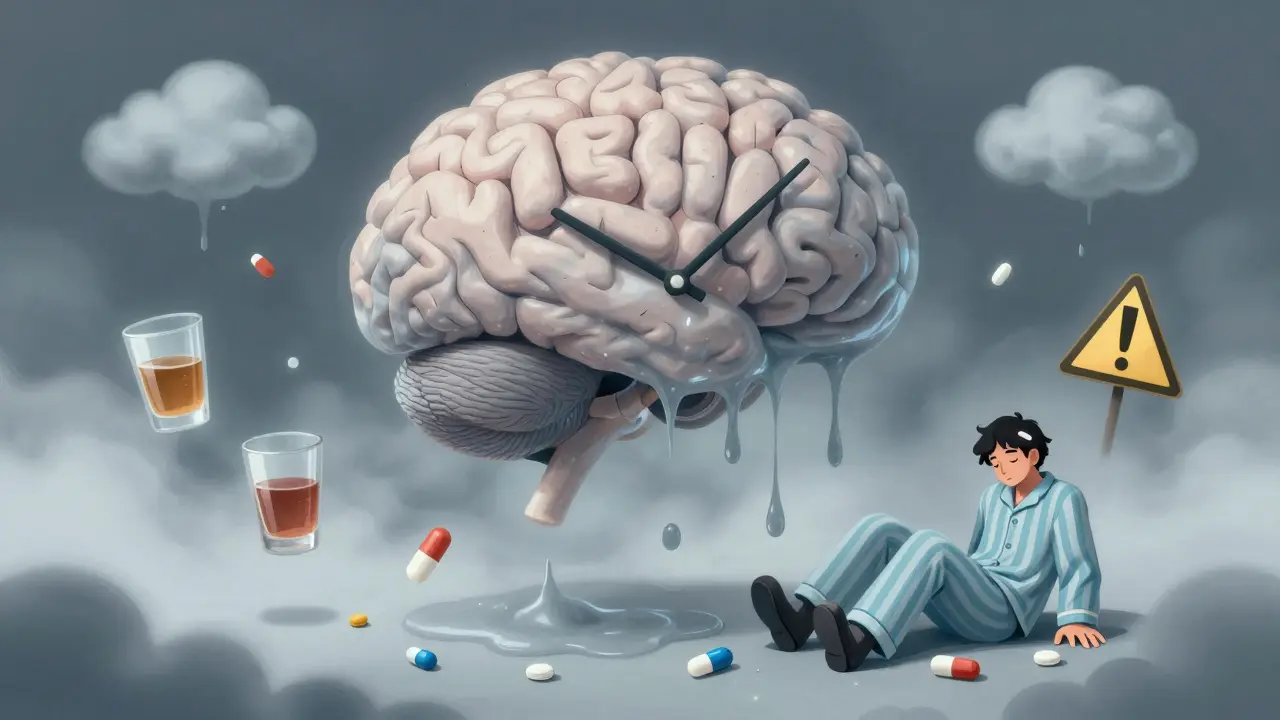
Why Managing These Side Effects Matters More Than You Think
It’s easy to think of these side effects as just part of the deal. But they’re not harmless inconveniences. They’re major reasons people stop taking opioids-or start misusing them. The CDC reports that more than two-thirds of people who misuse prescription opioids do so because they’re trying to relieve physical pain. If constipation is so bad you can’t leave the house, if drowsiness makes you useless at work, if nausea keeps you from eating-you might be tempted to take more than prescribed just to feel normal. Or worse, you might turn to street drugs. And if you suddenly stop opioids because the side effects are unbearable? That can trigger withdrawal: vomiting, diarrhea, sweating, anxiety, and intense pain. The FDA warns that abrupt discontinuation can lead to serious harm, including suicide. Managing side effects isn’t about comfort. It’s about safety. It’s about keeping you on the right treatment so you don’t end up in a worse place.What You Can Do Today
If you’re on opioids, here’s your action plan:- For constipation: Start a daily laxative regimen the same day you start opioids. Use a stimulant + osmotic combo. Drink 8-10 glasses of water daily. Walk for 20 minutes every day.
- For drowsiness: Take your dose at night. Avoid alcohol and sedatives. Review all other meds with your doctor. If you’re still foggy after two weeks, ask about a dose adjustment.
- For nausea: Don’t wait. Ask for an antiemetic on day one. If it doesn’t help in 3-5 days, try a different class. Consider switching to a different opioid if nausea persists.

When to Call Your Doctor
Not every side effect needs an emergency room. But some do. Call your doctor right away if you experience:- Not having a bowel movement for 4 or more days
- Severe drowsiness where you can’t stay awake or wake up easily
- Vomiting that lasts more than 24 hours or includes blood
- Confusion, slurred speech, or slow, shallow breathing
Can opioid-induced constipation ever go away on its own?
No. Unlike drowsiness or nausea, constipation doesn’t improve with time. Opioids permanently slow gut motility as long as you’re taking them. That’s why doctors recommend starting laxatives on day one. Waiting until you’re backed up makes it harder to fix.
Is it safe to take laxatives every day for years?
Yes, if they’re the right kind. Stimulant laxatives like senna and osmotic agents like polyethylene glycol are safe for long-term use under medical supervision. Avoid herbal laxatives or products with phenolphthalein, which can be harmful over time. Always follow your doctor’s dosage instructions.
Why do some people get nauseous from opioids and others don’t?
It varies by genetics, metabolism, and the specific opioid. Some people naturally have more sensitive chemoreceptor trigger zones in the brain. Others metabolize drugs differently. Tramadol and buprenorphine are generally less likely to cause nausea than oxycodone or morphine. Your doctor can choose a better fit based on your history.
Can I drive while taking opioids if I feel fine?
Don’t assume you’re safe just because you feel okay. Opioids can impair reaction time and judgment even when you don’t feel drowsy. Most experts recommend avoiding driving for the first week of treatment, and only resuming if you’ve been stable for weeks with no drowsiness or mental fog. Always check your state’s laws-some ban driving on opioids entirely.
What happens if I stop opioids suddenly because of side effects?
Stopping abruptly can trigger severe withdrawal: nausea, vomiting, diarrhea, muscle aches, anxiety, and intense pain. The FDA warns this can lead to uncontrolled pain, psychological distress, and even suicide. Always taper off slowly under medical supervision. Your doctor can create a plan to reduce your dose gradually while managing side effects.






9 Comments
I started opioids after my knee surgery and honestly didn’t know constipation was going to hit me like a freight train. My doctor gave me senna and MiraLAX on day one and it made all the difference. Just don’t wait until you’re stuck - it’s way harder to fix later.
/p>Also, drinking water like it’s your job helps. I went from 2 days between bowel movements to daily without even trying hard. Small wins, yknow?
Let’s be real here - the entire opioid paradigm is a pharmacological gamble dressed up as medicine. The fact that constipation is inevitable and untreated drowsiness leads to workplace accidents and potential fatalities speaks to a systemic failure in pain management culture. We’re treating symptoms with more chemicals while ignoring root causes like inflammation, nerve compression, and psychological distress. The CDC’s own data shows that 70% of misuse stems from unmanaged side effects - not addiction. That’s not addiction. That’s negligence wrapped in a prescription pad.
/p>And don’t get me started on the ‘just take laxatives’ advice. That’s like telling someone with a broken leg to just walk slower. It doesn’t fix the fracture. It just lets you limp longer while the system ignores the structural collapse.
Ugh I feel you. I was on oxycodone after my spine fusion and nausea had me crying in the bathroom at 3am. My nurse practitioner slipped me some Zofran and said ‘this isn’t weakness, this is biology’ - and that changed everything.
/p>Also, switching to buprenorphine was like swapping a sledgehammer for a scalpel. My brain didn’t feel like it was wrapped in wet socks anymore. Don’t suffer in silence - your doc wants you to feel human again, not just pain-free.
Drowsiness is real and no one talks about it enough. Took mine at night and it saved my job. No alcohol. No benzos. Just me and my pillow. If you're still foggy after two weeks talk to your doc. Simple. No drama. Just fix it./p>
THEY KNOW. THEY KNOW THIS IS HAPPENING. Why are they still pushing opioids like candy? It’s not medicine - it’s a corporate money machine. Big Pharma wrote the guidelines. The FDA is asleep. Your doctor gets kickbacks. Constipation? Drowsiness? Nausea? That’s just the side effect of the profit motive.
/p>I saw a guy on TikTok who went blind from opioid withdrawal. It’s not a coincidence. It’s a cover-up. They want you hooked. They want you dependent. They want you begging for more. Don’t trust the system. Fight back.
So let me get this straight - we’re telling people to take laxatives for the rest of their lives because Big Pharma made a drug that turns your guts into cement? And we call this ‘medicine’?
/p>Meanwhile my grandma takes a daily prune and calls it a day. Maybe we should’ve just stuck with that instead of inventing a chemical that turns humans into slow-motion zombies with blocked intestines.
Also, ‘start laxatives day one’? Sounds like the manual for a really aggressive customer retention strategy.
This post is gold. I’ve been on long-term opioids for fibromyalgia and this is exactly what I needed to hear. I was too embarrassed to ask about constipation - thought it was just ‘me being lazy.’ Turns out I just needed senna + MiraLAX. Life changed.
/p>Also, switching from morphine to buprenorphine cut my nausea by 80%. My doctor didn’t even blink. He said ‘let’s optimize.’ That’s the mindset we need - not guilt, not shame, just smart adjustments.
And yes - log your symptoms. I started a Notes app entry: ‘Opioid: 10mg, 8am. Nausea: 3/10. Bowel: 1/10. Energy: 2/10.’ My next appointment? I had data. They listened. That’s power.
Can we stop pretending this is just a medical issue? This is a cultural failure. We’ve turned pain into a problem that must be erased at all costs - even if it means turning people into constipated zombies who can’t drive or think. We don’t teach people how to live with pain anymore. We just drug them into oblivion.
/p>And now we’re surprised when they start misusing? Of course they do. If your life is defined by nausea and bowel emergencies, you’re going to chase anything that makes you feel normal. This isn’t addiction - it’s survival.
Also, if you’re from Canada or India and you think this is just an American problem, you’re delusional. The global pharmaceutical machine doesn’t care where you live. It just wants your prescription.
Wait - so the solution to opioids slowing your gut is to give you MORE drugs to un-slow it? Brilliant. We’re not treating pain anymore - we’re running a pharmacological circus. One pill to knock you out, two pills to un-knock your bowels, another to un-fog your brain, and a fourth to stop you from puking.
/p>Why not just… not take opioids? I mean, I get it - pain sucks. But is this really the only path? What about physical therapy? Acupuncture? CBD? Mindfulness? Or maybe - just maybe - we should stop pretending every ache needs a chemical override?
Also, if you’re taking laxatives for YEARS, aren’t you just training your colon to be lazy? Isn’t that the whole problem? We medicate the symptom and call it progress. Pathetic.