When it comes to slowing down vision loss from glaucoma, Dorzolamide Timolol has become a go‑to option for many eye doctors. This combination eye drop merges two proven mechanisms into one bottle, making it easier for patients to keep their eye pressure in check without juggling multiple prescriptions.
What is Glaucoma and Why Does Pressure Matter?
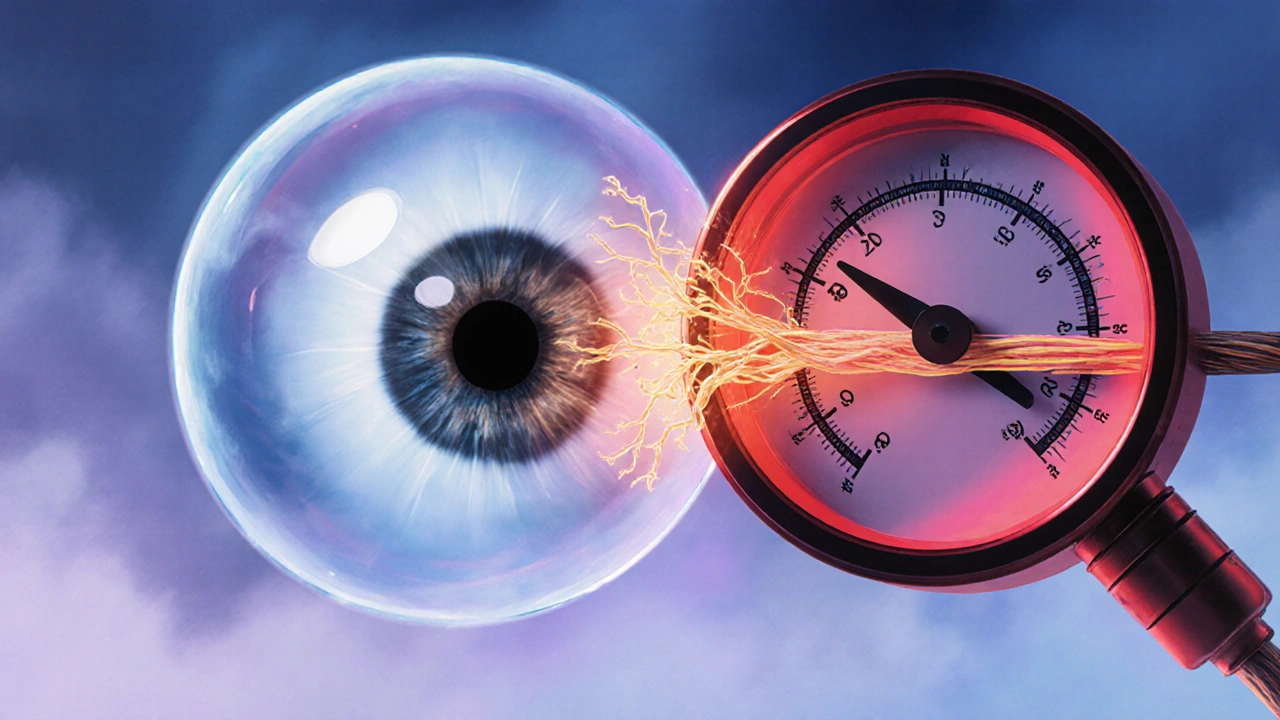
Glaucoma is a group of eye disorders that damage the optic nerve - the cable that carries visual information from the retina to the brain. The damage is usually linked to a rise in Intraocular Pressure (IOP), the fluid pressure inside the eye. When IOP climbs above the eye’s natural drainage capacity, the delicate nerve fibers begin to deteriorate, leading to peripheral vision loss that can eventually become total blindness if untreated.
Regular eye exams that include a visual field test and optic nerve imaging are the only way to catch the disease early, because glaucoma often progresses without noticeable symptoms.
How Dorzolamide‑Timolol Works: Two Drugs, One Goal
The power of this combo lies in its two active ingredients, each targeting aqueous humor production through a different pathway.
- Dorzolamide is a carbonic anhydrase inhibitor. It blocks the enzyme carbonic anhydrase in the ciliary body, reducing the amount of fluid the eye creates.
- Timolol belongs to the beta‑blocker class. By inhibiting beta‑adrenergic receptors, it also curtails fluid production.
When used together, the two agents cut aqueous humor output more than either could alone, delivering a larger IOP drop - typically 30‑35% from baseline in clinical trials.
Clinical Evidence: How Effective Is the Combo?
Several multicenter studies have measured the IOP‑lowering power of Dorzolamide‑Timolol versus its components used singly. A 2023 randomized trial involving 312 patients showed an average IOP reduction of 34% after 12 weeks of twice‑daily dosing, compared with 22% for Dorzolamide alone and 18% for Timolol alone. The combination also achieved target pressures (<18 mmHg) in 78% of participants, whereas monotherapies reached the same goal in roughly half of the cases.
Beyond numbers, the combo improves adherence. One survey of 150 glaucoma patients reported a 22% drop‑out rate for those on two separate drops, versus only 8% for those on the fixed‑dose Dorzolamide‑Timolol.

When to Use It: Patient Selection & Contra‑indications
Ideal candidates are adults with open‑angle glaucoma or ocular hypertension who need a stronger IOP‑lowering effect than a single agent can provide. It’s also beneficial for patients who have previously failed monotherapy or who struggle with the cost and inconvenience of multiple bottles.
Key contraindications include:
- Known sulfonamide allergy (risk with Dorzolamide)
- Severe asthma, chronic obstructive pulmonary disease, or bradycardia (caution with Timolol)
- Second‑ or third‑degree heart block without a pacemaker
Pregnant or nursing mothers should discuss risks with their ophthalmologist, as systemic absorption, though low, can affect the fetus.
How to Apply the Drops Properly
- Wash your hands thoroughly.
- Tilt your head back slightly and pull down the lower eyelid to create a small pocket.
- Hold the bottle close (no more than 2 cm) and gently squeeze one drop into the pocket. Avoid touching the tip to the eye or eyelashes.
- Close the eye gently for about 30 seconds - do not blink hard.
- If you use other eye medications, wait at least 5 minutes before applying the next drop.
Consistency matters. Missing doses can cause IOP spikes that undo weeks of progress. Setting a daily reminder on a phone or linking the dose to a regular activity (like brushing teeth) helps keep the schedule on track.
Comparing Dorzolamide‑Timolol with Other Glaucoma Therapies
| Drug Class | Mechanism | Typical IOP Reduction | Side‑Effect Profile | Best For |
|---|---|---|---|---|
| Dorzolamide‑Timolol | Carbonic anhydrase inhibitor + beta‑blocker | 30‑35% | Burning sensation, systemic beta‑blocker effects (rare) | Patients needing >20% IOP drop; who prefer single bottle |
| Prostaglandin analog (e.g., Latanoprost) | Increases uveoscleral outflow | 25‑30% | Darkening of iris, eyelash growth | First‑line therapy; good for once‑daily dosing |
| Alpha‑agonist (e.g., Brimonidine) | Decreases production & increases outflow | 15‑20% | Allergic conjunctivitis, dry mouth | Adjunct when prostaglandins insufficient |
| Selective laser trabeculoplasty (SLT) | Enhances trabecular meshwork drainage | 20‑30% (laser‑only) | Transient redness, mild discomfort | Patients reluctant to use daily drops |
While prostaglandin analogs remain the most frequently prescribed first‑line agents, Dorzolamide‑Timolol shines when a stronger, rapid IOP drop is needed without moving to laser or surgery.

Monitoring Success and Adjusting Therapy
After starting the combo, schedule a follow‑up within 4-6 weeks. The ophthalmologist will measure IOP, check for side effects, and possibly perform optic nerve imaging. If target pressure isn’t met, options include:
- Adding a prostaglandin analog (triple therapy)
- Switching to a fixed‑dose prostaglandin‑beta‑blocker combo
- Considering laser trabeculoplasty or minimally invasive glaucoma surgery (MIGS)
Tracking visual fields every 6-12 months also helps gauge whether the disease is truly being controlled.
Practical Tips to Maximize Benefits
- Store the bottle correctly: Keep it at room temperature, away from direct sunlight. Discard after 30 days of opening.
- Watch for systemic signs: If you notice unusual fatigue, shortness of breath, or a slow heartbeat, contact your doctor - timolol can be absorbed systemically.
- Don’t combine with certain nasal sprays: Some decongestants contain sympathomimetics that may counteract timolol’s effect.
- Use preservative‑free formulations if needed: Patients with dry eye or allergy may benefit from preservative‑free versions to reduce irritation.
Frequently Asked Questions
How quickly does Dorzolamide‑Timolol lower eye pressure?
Most patients see a measurable IOP drop within 30‑60 minutes after the first dose, with the full effect building over the first week of twice‑daily use.
Can I use Dorzolamide‑Timolol if I wear contact lenses?
It’s safest to remove contacts before applying the drops and wait at least 15 minutes before reinserting them. This prevents the medication from being trapped against the lens.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s less than 4 hours before the next scheduled dose. In that case, skip the missed one and resume your regular schedule - don’t double‑dose.
Are there any long‑term side effects?
Long‑term use is generally well tolerated. The most common complaints are mild eye irritation and a bitter taste. Systemic side effects from timolol are rare but can include lowered heart rate or bronchospasm in susceptible individuals.
How does the combo compare to prostaglandin eye drops?
Prostaglandins are often first‑line because they work once daily and have a low systemic impact. Dorzolamide‑Timolol provides a larger IOP reduction and is useful when a single prostaglandin isn’t enough or when a patient can’t tolerate its side effects (e.g., iris darkening).
Bottom line: Dorzolamide‑Timolol packs two proven mechanisms into a convenient bottle, delivering strong IOP control for many glaucoma patients. By understanding how it works, who it’s best for, and how to use it correctly, you can keep the pressure down and protect your vision.






10 Comments
Oh, great, another combo drop that pretends to be the miracle cure while we’re stuck with two bottles in one. The drama of “one bottle solves everything” is just marketing fluff.
/p>One must ask whether the industry’s relentless push for fixed‑dose combinations truly serves the patient or merely satisfies a profit‑driven narrative. The ethical implications are clear: convenience should never eclipse informed consent. Moreover, the data, while statistically significant, does not address individual variability in tolerance.
/p>When we contemplate the intricate dance of aqueous humor dynamics, we are confronted with a paradox of biology and pharmacology; the eye, a delicate organ, balances production and outflow with sublime precision. Dorzolamide, a carbonic anhydrase inhibitor, inserts itself into the enzymatic cascade, curbing the synthesis of bicarbonate and thereby diminishing aqueous production; this mechanistic elegance is not merely a chemical trick, but a manifestation of the body's inherent capacity for regulation. Timolol, on the other hand, engages beta‑adrenergic receptors, attenuating sympathetic stimulation and further reducing fluid generation-two distinct pathways converging upon a singular therapeutic goal. Clinical trials, such as the 2023 study involving 312 patients, demonstrate an average intraocular pressure reduction of 34% after twelve weeks; this figure, while impressive, must be contextualized within the broader spectrum of patient heterogeneity. Some individuals experience modest benefits, others achieve near‑target pressures; thus, personalization remains paramount. The side‑effect profile, though generally well‑tolerated, can include ocular irritation, a bitter taste, and systemic manifestations like bradycardia-a reminder that ocular pharmacology does not exist in isolation from systemic physiology. Moreover, the convenience of a single bottle must be weighed against the potential for reduced adherence if patients develop intolerance to either component. Long‑term data suggest stability in visual field preservation, yet the specter of progressive optic neuropathy looms for those inadequately controlled. In practice, the decision to employ Dorzolamide‑Timolol should be guided by a thorough baseline assessment, including baseline IOP, corneal health, and comorbid conditions such as asthma or COPD, where beta‑blockade could prove hazardous. Follow‑up within six weeks is advisable to confirm efficacy and monitor for adverse events; adjustments may involve adjunctive prostaglandin analogs or escalation to laser trabeculoplasty. Ultimately, the therapeutic narrative is not one of a panacea but of a strategic tool-effective when wielded with discernment, limited when applied without nuance.
/p>Listen, the whole "one bottle solves all" hype is just a marketing gimmick – it dont actually make the pressure drop any faster, its just two drugs in a single container, i mean cmon.
/p>😂
/p>It’s fascinating how a simple combination can spark such debate; the underlying science is solid, yet the conversation drifts into philosophy about patient autonomy and the nature of medical convenience.
/p>Dear community, I wish to emphasize that while the pharmacodynamics are well‑documented, the socioeconomic implications merit equal consideration; accessibility, insurance coverage, and educational outreach are integral to successful implementation.
/p>yo its cool but dont forget that some ppl cant stand the bitter taste and it can mess up your day.
/p>Honestly, if you’re looking for a magic bullet, you’ll be disappointed; this combo is just another rung on the ladder of incremental improvements.
/p>While I appreciate the nuanced view, I remain optimistic-focused adherence and regular monitoring often turn modest pressure drops into meaningful preservation of vision.
/p>