
When you’re scheduled for surgery, the last thing you want is a surprise reaction to a drug you’ve never even heard of. But every year, thousands of patients experience preventable complications because their past drug reactions weren’t clearly communicated. It’s not about being overly cautious-it’s about survival. A severe allergic reaction during anesthesia can turn a routine procedure into a life-or-death situation. The good news? You can stop that from happening with simple, clear steps.
Know Exactly What Happened to You
Many people say they’re "allergic" to a drug when they actually had a side effect. Nausea after codeine? That’s not an allergy. A rash after penicillin? That might be. Anaphylaxis-trouble breathing, swelling, low blood pressure-after rocuronium? That’s a true allergic reaction. The difference matters.Write down the exact drug name, what you felt, how long it took to start, and what helped. Did you break out in hives 10 minutes after the IV? Did your throat close up after morphine? Did you go into cardiac arrest after succinylcholine? Be specific. Vague answers like "I don’t like that medicine" won’t protect you.
Keep a list. Use your phone. Write it on a card. Carry it in your wallet. If you’ve ever had a reaction, even years ago, it still counts. Anesthesia drugs can trigger reactions you didn’t know you were vulnerable to.
Tell Everyone-Early and Often
Don’t wait until the day of surgery. Don’t assume your doctor already knows. Your primary care provider, surgeon, anesthesiologist, and pharmacist all need to hear it. And they need to hear it from you.Start with your surgeon’s office when you schedule the procedure. Ask for a pre-op medication review form. Fill it out completely. List every prescription, over-the-counter pill, vitamin, herbal supplement, and even recreational substance you’ve used in the last six months. Yes-even marijuana or CBD. Some drugs interact dangerously with anesthesia.
When you get to the hospital, repeat it. Tell the nurse who checks you in. Tell the anesthesiologist when they come to see you. Say it out loud: "I had a severe reaction to [drug name] in [year]. Here’s what happened." Don’t let them rush you. This isn’t a formality-it’s your safety net.
Use the Right Words
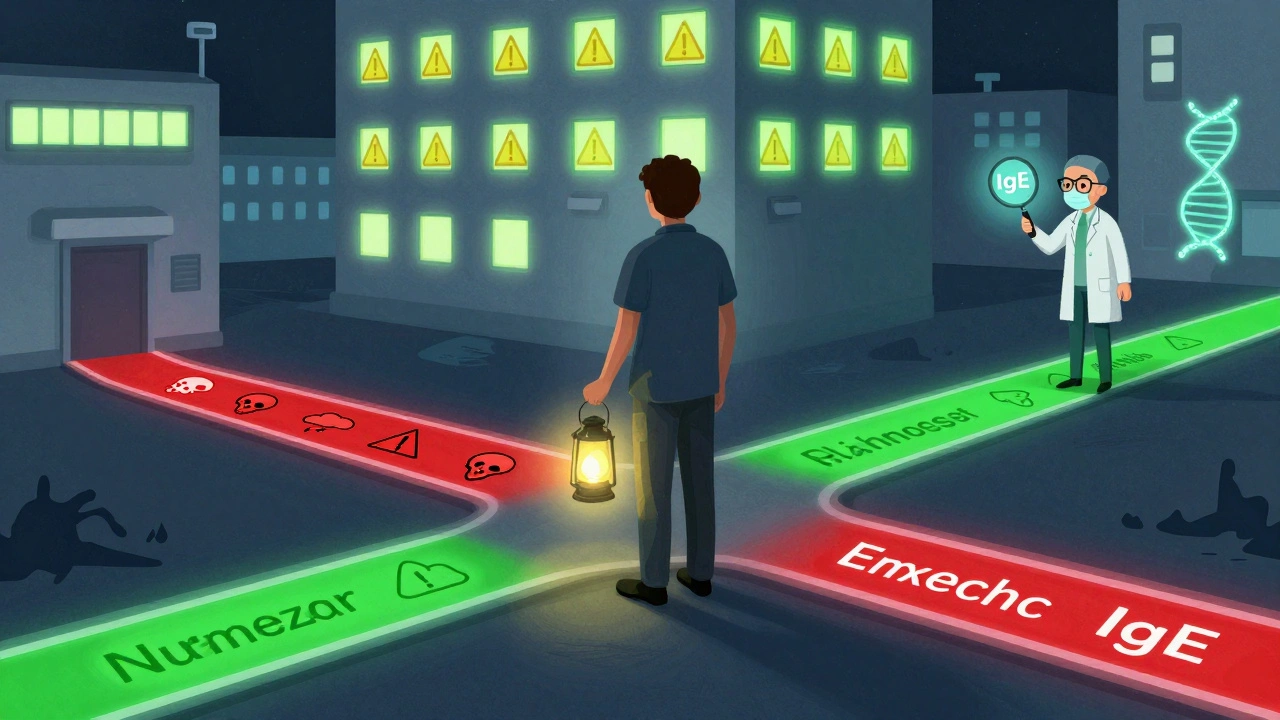
There’s a big difference between "I had a bad reaction" and "I had a true IgE-mediated allergic reaction." But you don’t need to know the medical jargon. Just describe what happened.For example:
- "After I got the IV for surgery, my face swelled up and I couldn’t breathe. They gave me epinephrine and I almost died. That was rocuronium."
- "I got a rash and fever after vancomycin. I was in the ICU for three days."
- "I felt dizzy and my heart raced after meperidine. I’ve never had that with any other painkiller."
These details help the team avoid not just the drug itself, but similar ones in the same class. If you reacted to rocuronium, they’ll avoid all neuromuscular blockers unless they’re certain it’s safe. If you reacted to codeine, they’ll skip all opioids metabolized by the same liver enzyme.
Ask for Documentation
Verbal warnings get lost. Paper or digital records don’t.Ask the hospital to add your reaction to your medical chart with the following details:
- Drug name (exact brand or generic)
- Reaction symptoms (include timing)
- Severity (mild, moderate, life-threatening)
- Treatment given
- Date of reaction
Request an allergy bracelet or card. Many hospitals offer them. If not, buy one online. Wear it. It’s your backup if you’re unconscious or can’t speak.
Also, ask if your hospital uses an electronic allergy alert system. Most do-Epic, Cerner, Meditech. But they only work if the info is entered correctly. Double-check it before signing any consent forms.
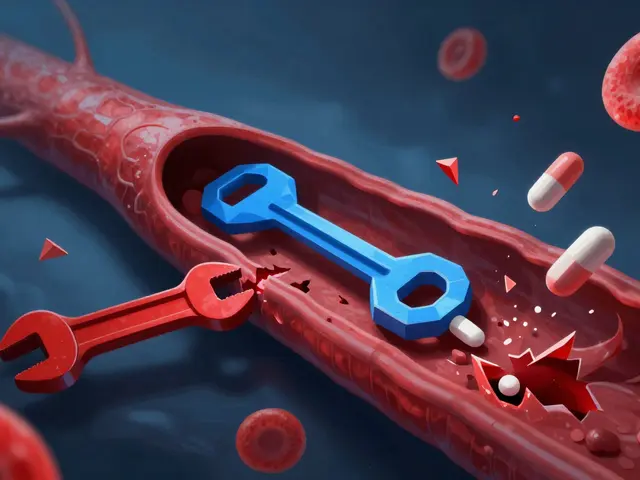
Know Which Drugs Are Riskiest
Some medications are far more likely to cause problems than others. Here are the top offenders during surgery:- Neuromuscular blockers (rocuronium, succinylcholine, vecuronium) - most common cause of anaphylaxis during anesthesia
- Antibiotics (vancomycin, penicillin, cephalosporins) - especially if you’ve had a rash or fever before
- Opioids (morphine, codeine, fentanyl) - can cause histamine release, leading to itching, flushing, or low blood pressure
- Latex - not a drug, but a common trigger. If you have eczema or spina bifida, you’re at higher risk
- Propofol - rare, but can cause severe reactions in people with egg or soy allergies (due to the emulsifier)
If you’ve ever reacted to any of these, flag them. Even if you think it was "just a side effect."
Don’t Assume Your Old Records Are Enough
Your family doctor’s chart might say "penicillin allergy"-but did they document the reaction? Was it confirmed by testing? If not, it’s just a note, not proof.Many hospitals now require allergy verification before surgery. That means they’ll ask you to describe the reaction in detail. If you can’t, they may refer you to an allergist for testing. Don’t wait until the day before surgery. Start this process weeks ahead.
If you’ve had a severe reaction, ask your doctor for a referral to an allergist. They can do skin tests or blood tests to confirm what you’re truly allergic to. This isn’t just for peace of mind-it changes your surgical plan. If you’re confirmed allergic to rocuronium, they can use a completely different muscle relaxant.
What If You Can’t Remember the Drug Name?
It happens. People forget. You might only remember the symptoms.Here’s how to work around it:
- "I had a reaction to something they gave me during surgery in 2018. I broke out in hives and my blood pressure dropped."
- "I got sick after every time I got anesthesia for dental work."
- "I was told I couldn’t have that drug again."
Even without the name, the pattern matters. The anesthesiologist can avoid entire drug classes based on your symptoms. They’ll choose safer alternatives.
Bring your old medical records if you have them. If you don’t, call the hospital where it happened. Most keep records for 10+ years.
What About Herbal Supplements and Vitamins?
Yes, they matter. St. John’s Wort can interfere with anesthesia. Garlic and ginkgo increase bleeding risk. High-dose vitamin E can thin your blood. Even fish oil can be a problem.Stop all supplements at least 7 days before surgery-unless your doctor says otherwise. Tell your team exactly what you take, how much, and how often. Don’t downplay them. They’re not "just natural."
What If You’re in an Emergency?
In emergencies, there’s no time for full screening. But that’s why documentation matters even more. If you’ve been hospitalized before, make sure your allergy history is in your chart. If you’re wearing a medical alert bracelet, it could save your life.Family members can help. If you’re unconscious, someone who knows your history should speak up. Give a trusted person a copy of your reaction list. Put it in your phone’s emergency contact info.
Why This Isn’t Just a "Formality"
A 2022 study found that 4.5% of surgical complications were linked to medication errors-and 1.1% of anesthesia-related deaths were caused by undiagnosed drug allergies. That’s not rare. That’s preventable.Hospitals that use standardized checklists and pharmacist reviews cut these errors by 37%. That’s not magic. That’s discipline. And it starts with you.
You’re not being difficult. You’re being smart. You’re the only person who knows your body’s history. No algorithm, no chart, no nurse can replace that.
Take 20 minutes before your surgery to write it down. Say it out loud. Make sure they write it down. It’s the most important thing you’ll do that day.
What if I don’t remember the name of the drug I reacted to?
You don’t need the exact name. Describe the reaction: what you felt, when it happened, and how severe it was. For example, "My face swelled up and I couldn’t breathe after an IV during surgery." That’s enough for the anesthesiologist to avoid entire classes of drugs. Bring old medical records if you have them, or call the hospital where it happened-they keep records for years.
Can I just tell the nurse on the day of surgery?
No. Waiting until the day of surgery is too late. Staff are rushed. Forms are filled out hours before. Your information might get lost or overlooked. Tell your surgeon’s office when you schedule the procedure. Follow up with your anesthesiologist at least a week before. Repeat it again when you arrive at the hospital.
Are herbal supplements really a risk?
Yes. St. John’s Wort can interfere with anesthesia drugs. Garlic, ginkgo, and high-dose vitamin E can increase bleeding. Fish oil can thin your blood. Even "natural" products can cause serious complications. Stop all supplements at least 7 days before surgery, and tell your team exactly what you take-even if you think it’s harmless.
What’s the difference between a side effect and an allergy?
A side effect is something unpleasant but not immune-related-like nausea from codeine. An allergy is when your immune system reacts, causing symptoms like hives, swelling, trouble breathing, or anaphylaxis. Anesthesiologists care more about true allergies because they can be deadly. But even side effects matter-they help them pick safer drugs.
Do I need to see an allergist before surgery?
If you’ve had a severe reaction-especially one involving breathing or low blood pressure-you should. An allergist can confirm what you’re allergic to with skin or blood tests. This lets your surgical team avoid not just the drug, but similar ones. It’s especially important if you’ve had reactions to muscle relaxants or antibiotics. Most hospitals recommend testing within 4-8 weeks after a reaction.
Can I get a medical alert bracelet?
Yes. Many hospitals offer them for free. If not, you can buy one online for under $20. Engrave it with your name, key allergies (e.g., "Allergic to rocuronium, vancomycin"), and emergency contact. Wear it at all times, especially before and after surgery. It’s your backup if you can’t speak.
What if my doctor says my reaction wasn’t serious?
You know your body better than anyone. If you felt like you were dying, it was serious-even if others didn’t. Insist on documenting it. Say, "I don’t care what they think-I’m not going through that again." Your safety is non-negotiable. If your doctor dismisses you, ask for a second opinion or request a referral to an anesthesiologist or allergist.



13 Comments
So let me get this straight-you’re telling me I need to memorize every drug I’ve ever been given like it’s a final exam, just so I don’t die on the table? Cool. I’ll just add it to my Tinder bio: ‘Looking for someone who won’t kill me with anesthesia. Also allergic to rocuronium.’
/p>Thank you for taking the time to outline these critical safety measures with such clarity. It is truly essential that patients understand the distinction between adverse effects and true immunological reactions. Proper documentation, early communication, and proactive collaboration with the surgical team can significantly reduce preventable morbidity and mortality. Your guidance is both practical and profoundly compassionate.
/p>good post! i had a bad reaction to morphine after knee surgery-swelling, itching, like 10 min after iv. i told the nurse but they didnt write it down. next time i printed a note and handed it to the anesthesiologist. saved my life. also, dont forget to mention if you’re allergic to latex-many gloves and tubes have it. and yes, even if you think it was ‘just a rash’-it counts. write it down, carry it, scream it if you have to.
/p>You people are ridiculous. If you can’t remember what drug you reacted to, you shouldn’t be allowed near a hospital. This isn’t a self-help blog-it’s medicine. If you’re too lazy to track your own medical history, maybe you deserve the consequences. Stop treating hospitals like customer service centers.
/p>There are at least seven grammatical errors in the original post. "Your" used instead of "you're." "Don't" contracted inconsistently. "There's" used with plural subjects. And why is "propofol" capitalized mid-sentence? If you're going to give life-or-death advice, at least proofread it.
/p>bro this is gold. i used to think "i hate that medicine" was enough. then my buddy went into anaphylaxis because they didn’t know he reacted to succinylcholine in 2016. he’s fine now, but wow. i made a note on my phone called "surgery survival" with all the drugs i’ve ever had issues with. even the dumb ones like that one time i got dizzy after a dental shot. you don’t need to be a doctor-you just need to be loud.
/p>It is deeply concerning that American patients are encouraged to treat medical professionals as if they are incapable of interpreting basic patient histories. In India, we have rigorous pre-op protocols, and patients do not need to carry laminated cards. This is a symptom of a broken healthcare system-overcompensating for incompetence with performative documentation. You are not a victim. You are a participant in a system that has been weakened by litigation and fear.
/p>Have you ever wondered why all these drug reactions keep happening? It’s not the patients. It’s the pharmaceutical companies. They test drugs on prisoners, then sell them to the public. The FDA is owned by Big Pharma. The anesthesiologists? They’re paid by the hospitals. The ‘allergy bracelet’? A scam. They want you to believe you’re safe so you’ll keep getting operated on. Wake up. Your body knows what’s killing you. Stop trusting the system.
/p>I read the whole thing and then forgot half of it. I think I had a bad reaction to something once but I’m not sure what. I’ll probably just wing it on surgery day. If I die, at least I didn’t waste time writing notes.
/p>you’re right-it’s not just about the drugs, it’s about being heard. i remember when i had my surgery and the anesthesiologist kept scrolling through his phone while i tried to explain the rash i got after penicillin as a kid. i just started crying. he stopped. listened. wrote it down. i’m alive because i refused to be quiet. if you’ve ever felt dismissed-don’t stop talking. your voice is the only thing standing between you and a nightmare.
/p>While your post is superficially useful, it lacks a foundational understanding of pharmacokinetic pathways and IgE-mediated hypersensitivity mechanisms. The assertion that "vague answers won’t protect you" is correct, yet you fail to emphasize the necessity of HLA typing for severe cutaneous reactions or the role of basophil activation tests in diagnosing non-IgE-mediated anaphylaxis. This is amateurish risk management dressed up as patient empowerment.
/p>thank you for this. i’m from india and we don’t talk about this enough. my cousin almost died because they gave her ceftriaxone after she said "i get rashes sometimes"-they didn’t ask for details. now she carries a small card in her purse with the exact drug, the date, and how her lips swelled like a balloon. i made one for my mom too. even if you think it’s not a big deal, it is. and if you’re scared to speak up? say it like you’re yelling at a waiter who got your order wrong. loud. clear. no apologies. your life isn’t a suggestion.
/p>Okay, so let me get this straight: you’re saying that if I say "I had a reaction," and the doctor doesn’t write it down in triplicate, with a notarized affidavit, and a QR code linking to my medical journal, then I’m basically signing my own death warrant? And if I forget to mention that I took a gummy vitamin with vitamin E last Tuesday, I’ll spontaneously combust under the scalpel? I love how this post turns every surgery into a spy movie where the only thing keeping me alive is my ability to recite a 17-item drug list from memory.
/p>