Buprenorphine for Withdrawal: What Works, What Doesn’t, and What to Expect
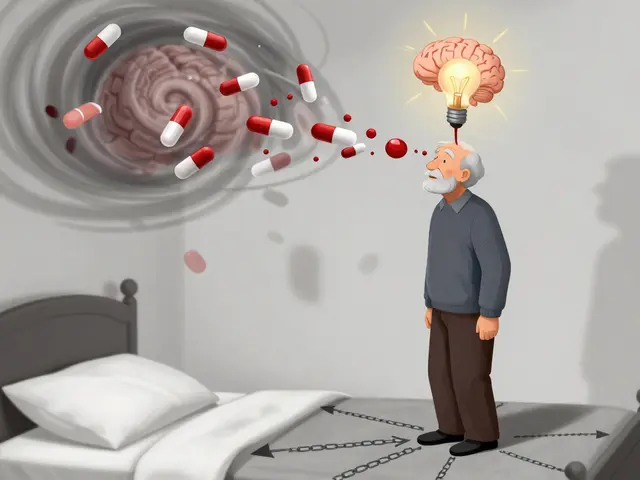
When someone stops using opioids, the body reacts hard—sweating, shaking, nausea, anxiety, and intense cravings. That’s where buprenorphine for withdrawal, a partial opioid agonist used to manage opioid dependence and reduce withdrawal symptoms. Also known as Suboxone (when combined with naloxone), it helps stabilize the brain without causing the same high as full opioids. Unlike methadone, which fully activates opioid receptors, buprenorphine only partly turns them on. That means less risk of overdose, fewer side effects, and a smoother transition off drugs.
It’s not magic, but it’s one of the most reliable tools doctors use today. People who use buprenorphine for withdrawal report less muscle pain, fewer stomach cramps, and reduced anxiety compared to going cold turkey. It doesn’t erase withdrawal overnight, but it cuts the worst of it by 60-80%. Many start it in a clinic, under supervision, then switch to take-home doses. The key is timing: starting too early can trigger sudden withdrawal; starting too late means suffering longer than needed. Most providers wait until mild symptoms appear—usually 12 to 24 hours after the last opioid dose.
It’s not just about the drug itself. Success depends on support, routine, and mindset. People who combine buprenorphine with counseling, group meetings, or even just a daily check-in with a friend do better long-term. It’s not a cure, but it’s a bridge—giving you the physical stability to rebuild your life. You can’t just take it and forget about it. You still need to address the habits, triggers, and emotional pain that led to use in the first place.
Some people worry it’s just swapping one drug for another. But that’s not how it works. Buprenorphine doesn’t produce euphoria at maintenance doses. It doesn’t make you high. It just takes the edge off. Think of it like insulin for diabetes—you don’t get a sugar rush from insulin, but you avoid the chaos of uncontrolled blood sugar. Same here.
It also works well with other treatments. You’ll see posts here comparing it to naltrexone, methadone, and even non-opioid options like clonidine or gabapentin for specific symptoms. Some use it short-term to get through detox. Others stay on it for months or years. There’s no one-size-fits-all timeline. What matters is what works for you.
What you’ll find in the posts below are real comparisons, user experiences, and clinical insights on how buprenorphine fits into the bigger picture of opioid recovery. You’ll see how it stacks up against other meds, what side effects actually happen, how to talk to your doctor about it, and what to avoid when you’re trying to get clean. No fluff. No hype. Just what works—and what doesn’t—when you’re trying to get your life back.
Opioid Withdrawal Timeline and How to Manage Symptoms Safely
Learn the opioid withdrawal timeline and proven strategies to manage symptoms safely. Discover how medications like buprenorphine, hydration, and medical supervision improve recovery outcomes.