Emotional Impact: How Illness and Meds Affect Feelings
Feeling overwhelmed by sickness or a new medication is normal. Physical health and emotions are tied together. A diagnosis, daily side effects, or long recovery can change moods, make you anxious, or sap motivation.
Short-term reactions vary. Some people feel angry or sad after a diagnosis. Others notice sleep shifts or strange dreams when starting antidepressants. Side effects like fatigue and headaches can lower patience and make social life harder. Even minor conditions that affect appearance, like hair loss from treatment, can hit confidence.
Chronic illness brings a different load. When treatment is ongoing, worry about the future becomes constant. Daily meds, doctor's visits, and limits on activities can lead to low mood or burnout. Friends and family might not see the small daily costs, which makes you feel isolated. That gap between how you look and how you feel often adds stress.
Medications can directly change emotions. Drugs that alter neurotransmitters sometimes cause mood swings, vivid dreams, or numbness. Steroids may create jitteriness or short temper. Blood pressure drugs can make people feel tired and less driven. If your feelings change soon after starting a medicine, talk with your clinician before stopping it.
Practical steps that help day to day:
- Track changes. Keep a short journal of mood, sleep, and side effects for two weeks. It makes patterns clear.
- Prioritize sleep. Small wins like a consistent bedtime and reduced screen time improve mood.
- Move a bit. Short walks or simple stretching reduce stress chemicals and boost energy.
- Share one specific need with someone close. Saying “I need a 10‑minute check‑in” makes support real.
- Ask about medication swaps or dose changes if side effects hurt your life.
When to ask for professional help:
- Suicidal thoughts, severe hopelessness, or inability to function require immediate contact with a clinician or crisis service.
- If mood changes are severe or last more than two weeks, book a medical review.
- For sleep or dream problems tied to antidepressants, your prescriber can adjust timing or switch drugs.
Communicating well with your healthcare team helps. Bring your notes, describe exact timing of changes, and say how feelings affect daily tasks. Ask what to expect next and what alternatives exist. A clear list of questions avoids forgotten points.
Small practical tools can ease the load. Use reminder apps for meds so you worry less. Try brief breathing exercises during flares. Look for local support groups or online forums focused on your condition and reading other people’s real experiences often helps.
You don’t have to accept feeling worse as part of treatment. With tracking, honest talk, and a few simple routines, many people regain emotional balance while managing physical health.
Want examples? Check our articles on lupus and pregnancy, antidepressant dreams, and bacterial eye infections to read real cases and practical tips. Use those pages to prepare specific questions for your clinician. If you need one simple start, track mood and do a two‑minute breathing practice each day for two weeks.
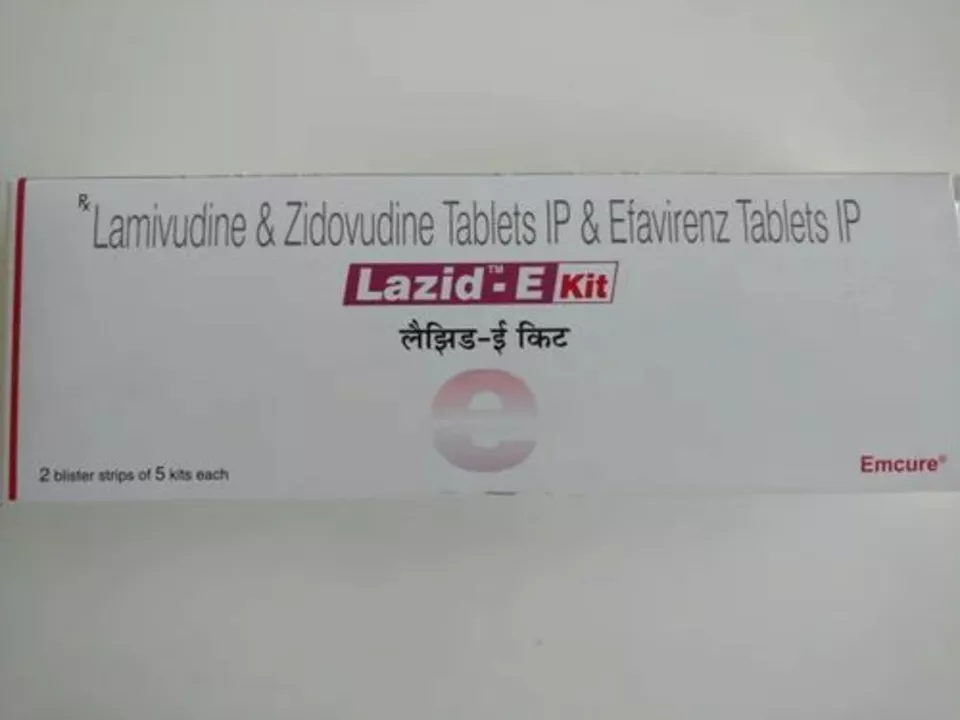
Lamivudine-Zidovudine and Mental Health: Managing the Emotional Impact of HIV
As someone living with HIV, managing my mental health is a crucial aspect of my holistic well-being. Lamivudine-Zidovudine is an important treatment that helps keep the virus at bay, but it's essential to also address the emotional impact of the diagnosis. I've learned that seeking support from therapists, support groups, and loved ones is vital for coping with the challenges and maintaining a positive outlook. Additionally, practicing self-care and stress management techniques has helped me improve my overall mental health. By prioritizing both my physical and emotional well-being, I am better equipped to navigate life with HIV.