FDA Generic: What You Need to Know About Safe, Affordable Medications
When you pick up a FDA generic, a medication approved by the U.S. Food and Drug Administration as equivalent to a brand-name drug in dosage, strength, and performance. Also known as generic drugs, it is the most common way people save money on prescriptions without sacrificing effectiveness. But here’s the thing: FDA generic doesn’t mean identical. It means bioequivalent—meaning it delivers the same active ingredient at the same rate and amount as the brand. That’s the law. But what’s inside the pill beyond the active drug? That’s where things get messy.
Every pill has inactive ingredients—fillers, dyes, preservatives, lactose, gluten. These are called excipients in generics, non-active substances used to bind, stabilize, or color a medication. They don’t treat your condition. But for some people, they cause real problems: stomach upset, rashes, bloating, even allergic reactions. A generic version of your blood pressure pill might use a different dye than the brand. That’s legal. But if you’re sensitive to Red 40? You might not know why you feel off. And no one tells you this when you fill the prescription.
Then there’s the science behind approval. The FDA doesn’t test every single batch of every generic. Instead, they rely on replicate study designs, advanced clinical methods used to prove a generic drug behaves the same as the original, especially for drugs with highly variable absorption. These studies are complex, expensive, and often done with small groups. Some drugs—like blood thinners, thyroid meds, or seizure drugs—are so sensitive that tiny differences in how they’re absorbed can change how well they work. That’s why your doctor might stick with the brand for those.
And here’s something most people don’t realize: a generic drug can be made in a different country, under different inspection standards. The FDA inspects foreign factories, but not every one, every time. Some generic makers have been caught cutting corners—using substandard ingredients, falsifying data. It’s rare, but it happens. And when it does, recalls follow. You might never know if your pills came from a factory with a clean record or one that got slapped with a warning letter.
So what should you do? Don’t assume all generics are the same. If you’ve had a bad reaction to a generic, write down the name, the manufacturer, and what happened. Bring it to your pharmacist. Ask: "Is this the same maker as last time?" Ask about excipients. Ask if there’s another generic version available. And if you’re on a critical drug—like warfarin, levothyroxine, or theophylline—stick with the same brand or same generic maker unless your doctor says otherwise.
The truth? FDA generic saves millions of dollars every year. It’s not a compromise—it’s a smart choice. But it’s not magic. You still need to pay attention. Your body doesn’t care about the label. It cares about what’s in the pill. And sometimes, that’s the difference between feeling fine and feeling awful.
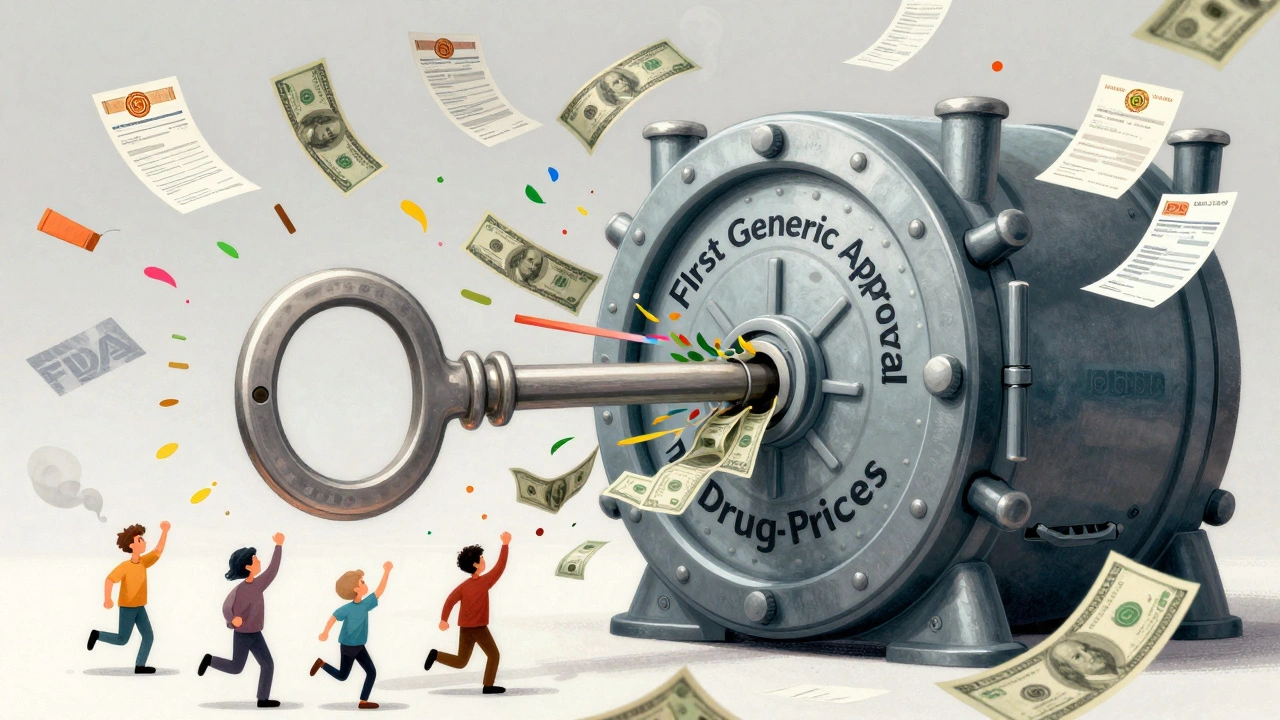
First Generic Approval: Why It Matters and What It Means for Your Prescription Costs
First generic approval is the key to lowering drug prices in the U.S. It gives the first company to launch a generic version of a brand-name drug 180 days of exclusive sales-leading to massive cost savings for patients and the healthcare system.