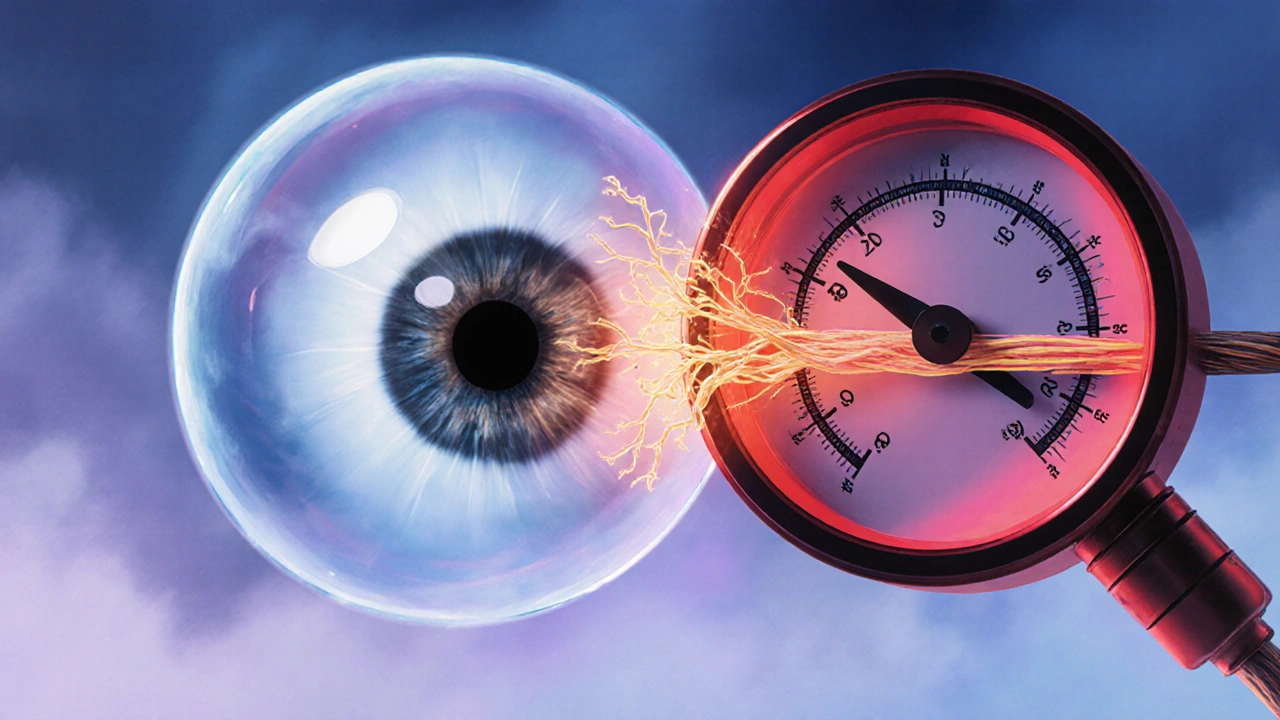
Intraocular Pressure: What It Is and Why It Matters
When dealing with Intraocular Pressure, the fluid pressure inside the eye that keeps its shape and supports visual function. Also known as IOP, it plays a critical role in eye health. Elevated IOP can damage the optic nerve and lead to vision loss. Glaucoma, a group of eye diseases characterized by progressive optic nerve damage often starts with high IOP. To check the pressure, eye doctors use Tonometry, a quick, painless test that measures the eye’s internal pressure. If the numbers are too high, Prostaglandin analogs, medications that increase fluid outflow to lower eye pressure are a common first‑line therapy. Understanding these basics sets the stage for smarter decisions about eye care.
How Intraocular Pressure Is Measured and Interpreted
Tonometry comes in several flavors – applanation, non‑contact “air‑puff,” and handheld devices – but they all aim to give a reliable intraocular pressure reading in millimeters of mercury (mm Hg). Normal ranges sit between 10 and 21 mm Hg; values above this window signal ocular hypertension, a warning sign that glaucoma may develop if untreated. The test is quick, usually done during a routine eye exam, and the results help doctors decide whether medication, laser therapy, or surgery is needed. Knowing your own pressure trend is useful because IOP can fluctuate throughout the day, and a single high reading doesn’t always mean trouble, just that you should be monitored.
Beyond the numbers, doctors look at risk factors such as family history, age, and corneal thickness. Thin corneas can underestimate true pressure, while thick corneas may over‑estimate it. This is why a comprehensive eye exam often pairs tonometry with imaging of the optic nerve and visual field testing. Together, these assessments paint a clear picture of how the pressure is affecting the eye’s structure and function.
When pressure is too high, treatment options focus on either reducing fluid production or improving outflow. Prostaglandin analogs, like latanoprost, are favored because they work once daily and have a strong safety record. Beta‑blockers, alpha‑agonists, and carbonic anhydrase inhibitors are other drug classes that target different pathways. In some cases, laser procedures such as selective laser trabeculoplasty (SLT) can boost drainage without medication. Surgery, though less common, becomes an option when drugs and lasers don’t achieve target pressures.
Living with elevated intraocular pressure means staying on top of follow‑up appointments and adhering to prescribed drops. Missing doses can cause pressure spikes that damage the optic nerve silently. Lifestyle tweaks—like regular exercise, a balanced diet low in caffeine, and managing systemic blood pressure—can also support eye health. Patients often report that understanding why they need each medication makes them more diligent about usage.
The articles below dive deeper into specific drugs, measurement techniques, and management strategies related to intraocular pressure. Whether you’re searching for the latest on prostaglandin analogs, comparing tonometry devices, or looking for tips on handling ocular hypertension, you’ll find practical insights to help you keep your eyes healthy.
Dorzolamide‑Timolol for Glaucoma: How It Works, Benefits & Use
Discover how Dorzolamide‑Timolol works, its benefits for glaucoma, dosing tips, side effects, and how it stacks up against other eye drops.