Understanding Dementia of the Alzheimer's Type
Dementia of the Alzheimer's type is a progressive, degenerative neurological disorder that affects the memory, cognitive abilities, and personality of the individual. It is the most common cause of dementia in the elderly and is characterized by the gradual decline in cognitive functions, affecting memory, reasoning, language, and problem-solving abilities. As the disease progresses, it becomes increasingly difficult for individuals to perform daily tasks, maintain social relationships, and live independently. In this article, we will discuss the importance of social interaction in managing dementia of the Alzheimer's type, and how it can help improve the quality of life for affected individuals and their caregivers.
The Importance of Social Interaction
Social interaction is essential to our overall well-being and plays a crucial role in maintaining our mental health. It helps to keep our minds active, provides a sense of belonging, and reduces feelings of isolation and loneliness. For individuals with dementia of the Alzheimer's type, social interaction is even more critical as it can help slow down the progression of cognitive decline and improve their overall quality of life. Engaging in meaningful social activities can help individuals with dementia maintain their sense of identity, feel more connected to others, and stimulate their cognitive abilities.
Barriers to Social Interaction
Individuals with dementia of the Alzheimer's type often face various barriers to social interaction. These barriers can be both internal, such as the cognitive and emotional challenges associated with the disease, and external, such as the stigma and misunderstandings surrounding dementia. Some common barriers include communication difficulties, memory loss, apathy, and reduced social skills. Additionally, caregivers may be unsure of how to facilitate social interactions for their loved ones with dementia or may be overwhelmed by their caregiving responsibilities.
Strategies to Enhance Social Interaction
There are several strategies that caregivers can implement to enhance social interaction for individuals with dementia of the Alzheimer's type. These strategies include creating a supportive environment, encouraging participation in meaningful activities, maintaining familiar routines, and promoting effective communication. By providing opportunities for social engagement and supporting individuals with dementia in their social interactions, caregivers can help improve their loved ones' cognitive functioning and emotional well-being.
Group Activities for Social Engagement
Participating in group activities can be an effective way to promote social engagement for individuals with dementia of the Alzheimer's type. Group activities should be tailored to the individual's interests, abilities, and cognitive functioning. Some examples of group activities include art therapy, music therapy, reminiscence groups, and exercise classes. These activities can provide individuals with dementia the opportunity to connect with others, share experiences, and maintain a sense of purpose and belonging.
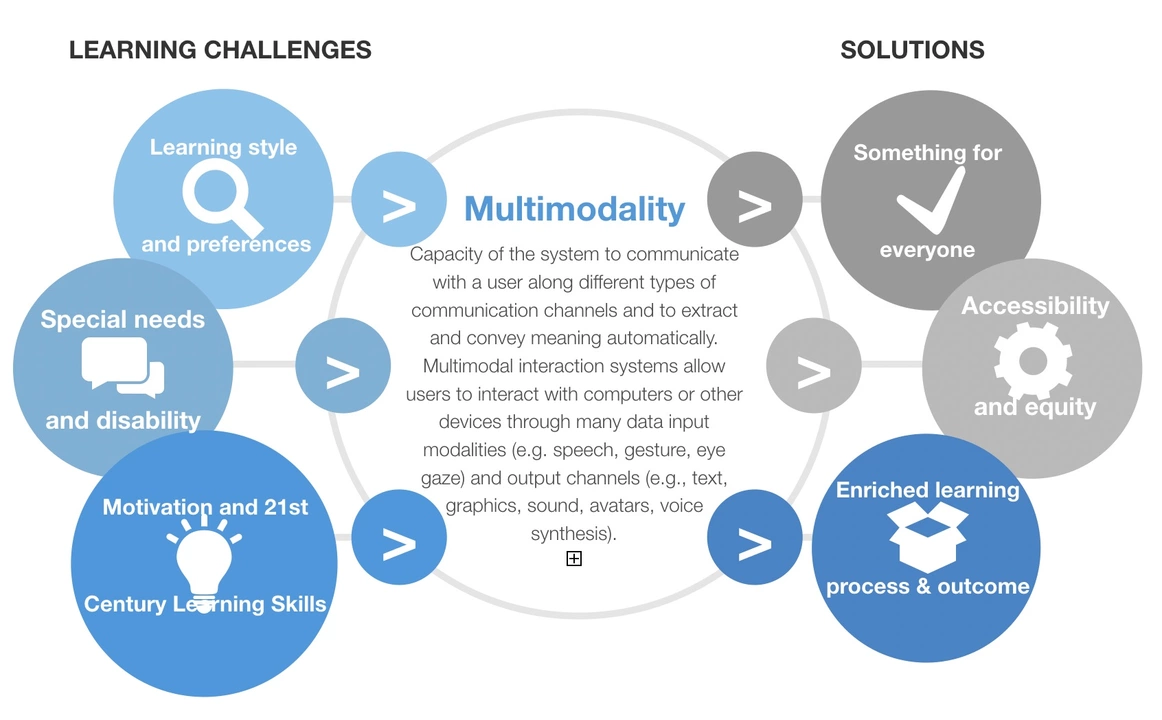
Technology and Social Interaction
Technology can play a significant role in facilitating social interaction for individuals with dementia of the Alzheimer's type. Social media platforms, video conferencing tools, and online support groups can help individuals with dementia stay connected with friends and family members, even if they are geographically distant. Additionally, digital games and cognitive training apps can provide cognitive stimulation and opportunities for social engagement. Caregivers should be mindful of the potential risks associated with technology use, such as privacy concerns and online scams, and provide appropriate guidance and supervision.
Role of Community and Social Support
Community resources and social support networks play a vital role in promoting social interaction for individuals with dementia of the Alzheimer's type. Local community centers, senior centers, and memory cafes can offer social activities, support groups, and educational programs for individuals with dementia and their caregivers. Involvement in these community resources can help reduce feelings of isolation and provide individuals with dementia and their caregivers with valuable social connections and support.
Conclusion
In conclusion, social interaction is a crucial aspect of managing dementia of the Alzheimer's type. By fostering social connections, promoting engagement in meaningful activities, and utilizing community resources and technology, caregivers can help improve the quality of life for individuals with dementia and support their cognitive functioning and emotional well-being. Ultimately, a strong network of social support can make a significant difference in the lives of those affected by dementia of the Alzheimer's type.






14 Comments
Social circles can act like a gentle buffer against the fog of memory loss.
/p>Keeping a routine of coffee chats or short walks often keeps the mind humming.
Too many buzzwords; the article glosses over the fact that not every group activity is feasible for advanced patients.
/p>Mixing music with reminiscence sessions can spark old stories and sharpen recall.
/p>A simple playlist of 60s hits often does the trick.
Ensure lighting is adequate during group sessions to reduce visual confusion.
/p>Training caregivers on how to cue conversation topics can make interactions feel less forced.
/p>Setting up a weekly "memory box" with photos, letters, and keepsakes gives concrete prompts.
Encouraging participation in low‑stress hobbies like knitting or gardening lets patients stay active without overwhelming them.
Pairing these activities with a familiar caregiver presence builds confidence and reduces anxiety.
Ultimately, consistency and personalization are the cornerstones of successful social engagement.
It is incumbent upon us, as custodians of public health, to scrutinize the purported benefits of social interaction with a judicious eye.
/p>While extant literature extols the virtues of communal engagement for individuals afflicted with Alzheimer’s disease, such commendations are oft‑laden with methodological laxities.
One must first consider the heterogeneity of patient cohorts, whose cognitive baselines differ vastly across studies.
Second, the purported mechanisms-ranging from neuroplasticity to psychosocial reinforcement-remain speculative in the absence of rigorous neuroimaging corroboration.
Third, the deployment of technology as a conduit for connection introduces vectors of privacy erosion that are insufficiently addressed by current regulatory frameworks.
Moreover, the commercialization of remote interaction platforms has cultivated a lucrative market that may prioritize profit over patient welfare.
This confluence of profit motives and lax oversight creates fertile ground for exploitation under the guise of therapeutic innovation.
Consequently, caregivers must remain vigilant against spurious claims that promise miracle improvements through mere conversation.
An evidence‑based approach demands randomized controlled trials with transparent inclusion criteria and long‑term follow‑up.
Such trials should also quantify adverse outcomes, including increased agitation or caregiver burnout resultant from poorly structured activities.
Only through such stringent scrutiny can we distinguish genuine therapeutic value from anecdotal optimism.
Until such standards are universally adopted, the integration of social interaction into care plans should be approached with calibrated skepticism.
Healthcare providers ought to counsel families about realistic expectations, emphasizing that social engagement complements, rather than supplants, pharmacological regimens.
In addition, policy makers should allocate resources toward training programs that empower caregivers to facilitate meaningful and safe interactions.
Finally, a collective commitment to transparency and scientific rigor will safeguard the dignity of those navigating the harrowing landscape of Alzheimer's disease.
The tapestry of human connection weaves a subtle pattern that can illuminate even the dimmest corridors of a fading mind.
/p>When we share stories, we are not merely exchanging words; we are handing over fragments of identity that anchor the self.
Thus, a well‑timed joke or a familiar song becomes a lighthouse in the tempest of confusion.
Crafting such moments demands patience, empathy, and a dash of creative flair.
Creative cues work wonders when they’re simple and familiar.
/p>Use everyday objects to spark conversation without overcomplicating the scene.
Imagine a room alive with the soft hum of a grand piano, each note coaxing forgotten memories to the surface.
/p>The scent of fresh‑baked bread wafts in, reminding everyone of Sunday mornings spent around the kitchen table.
These sensory threads, when woven together, create a vivid tapestry that can briefly lift the veil of dementia.
Yet, the drama lies in the balance-too much stimulus can tip into overwhelm, so moderation is key.
Mindful orchestration, therefore, becomes the unsung hero of meaningful engagement.
Proper cueing reduces confusion.
/p>Across cultures, communal storytelling has long served as a vessel for memory preservation.
/p>Recognizing this can guide us toward more inclusive activity designs.
In practice, integrating cultural motifs-such as regional folk songs or traditional games-enhances relevance and encourages participation.
/p>When caregivers respect and reflect a participant’s heritage, the sense of belonging deepens, potentially mitigating the isolation often reported in dementia care.
Great points everyone.
/p>Let’s keep sharing practical tips and remember to celebrate the small victories each day brings.
From a systems‑engineering perspective, deploying interoperable platforms that synchronize caregiver schedules with patient activity logs can drastically reduce coordination latency.
/p>Ensuring API compliance with HIPAA standards further safeguards data integrity while enabling real‑time feedback loops.