Hatch-Waxman Act: How Generic Drugs Got Approved and Changed Medication Access
When you pick up a generic pill at the pharmacy, you’re seeing the result of the Hatch-Waxman Act, a 1984 U.S. law that created the modern pathway for generic drug approval. Also known as the Drug Price Competition and Patent Term Restoration Act, it’s the reason you can buy the same medicine as a brand-name drug for a fraction of the cost. Before this law, generic makers had to repeat expensive clinical trials just to prove their drug worked—something brand-name companies had already done. That made generics too costly to produce, and most patients couldn’t afford the originals.
The Hatch-Waxman Act changed that by letting generic companies prove their drugs were bioequivalent, meaning they delivered the same amount of active ingredient into the bloodstream at the same rate as the brand version. No need for new human trials. Just solid lab data. At the same time, it gave brand-name drug makers extra patent time—up to five years—to make up for the time lost during FDA review. This wasn’t a giveaway; it was a trade. Innovation got protected. Competition got enabled.
That trade created a system where generics could enter the market as soon as patents expired or were challenged. It’s why you now see multiple versions of drugs like Lipitor, Nexium, or Humira at different prices. But it’s not perfect. Some companies game the system by filing endless minor patent extensions, delaying generics. Others make tiny changes to the drug’s formulation to avoid generic competition—something you might notice if your generic suddenly feels different. That’s where excipients in generics, the inactive ingredients like fillers or dyes come in. They don’t affect how the drug works, but they can cause reactions in sensitive people. And that’s why some patients stick with brand names—not because they’re better, but because they’re more predictable.
The Hatch-Waxman Act also laid the groundwork for how the FDA evaluates replicate study designs, a method used to test highly variable drugs where standard bioequivalence rules don’t work. If a drug’s absorption changes too much from person to person—like some blood thinners or epilepsy meds—the FDA needs smarter ways to prove generics match. That’s why you see complex study designs in the background of every generic approval, even if you never see them on the label.
Today, over 90% of prescriptions in the U.S. are filled with generics. That’s not an accident. It’s the direct result of this law. But the system is under pressure. Biosimilars, complex biologic drugs that aren’t exact copies, are now entering the market—and they don’t fit neatly into the Hatch-Waxman framework. The FDA is still figuring out how to handle them. Meanwhile, patients still get confused when their generic switches brands, or when a drug they’ve been taking for years suddenly costs more. The Hatch-Waxman Act didn’t solve everything. But it made sure that for most people, getting the medicine they need doesn’t mean going broke.
Below, you’ll find real-world stories and science behind how this law affects your prescriptions—from drug interactions and dosing quirks to why your generic might taste different. It’s not just policy. It’s your medicine.
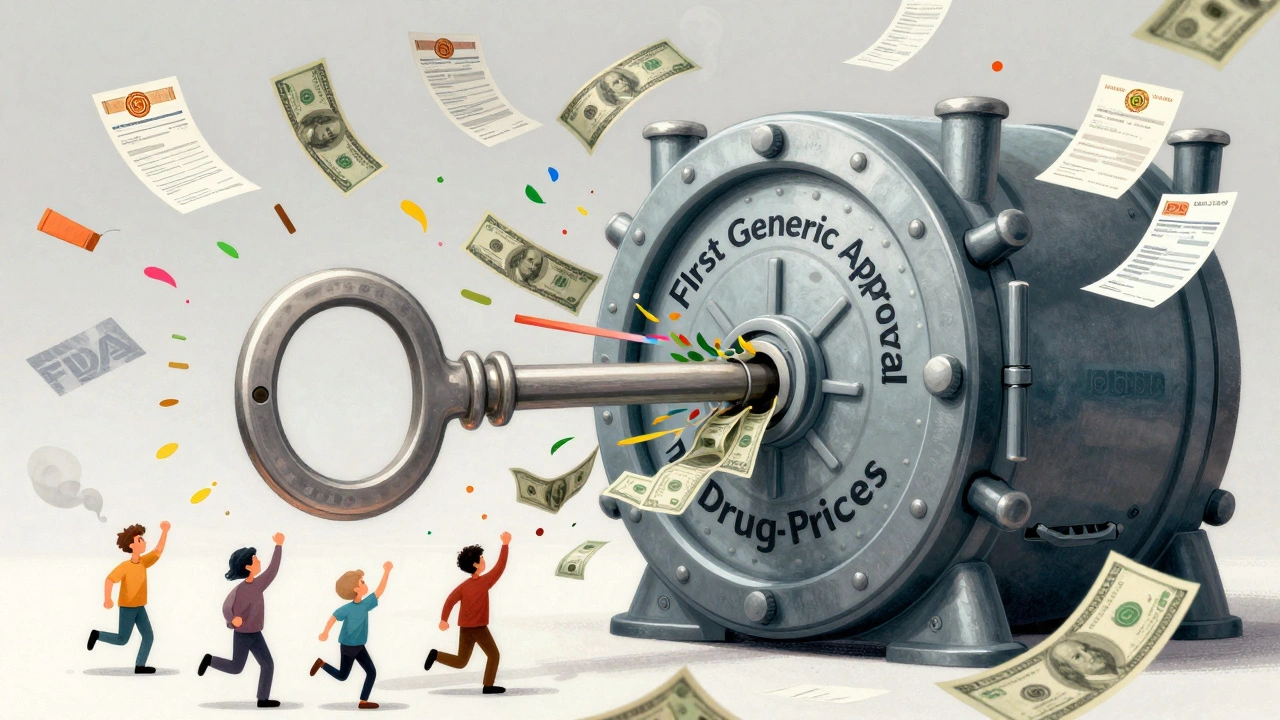
First Generic Approval: Why It Matters and What It Means for Your Prescription Costs
First generic approval is the key to lowering drug prices in the U.S. It gives the first company to launch a generic version of a brand-name drug 180 days of exclusive sales-leading to massive cost savings for patients and the healthcare system.