Eye Drops: A Practical Guide to Ophthalmic Medications
When working with Eye Drops, topical liquid medicines applied directly to the eye surface to treat or prevent ocular conditions. Also known as ophthalmic drops, they are a convenient way to deliver drugs where they’re needed most. Ophthalmic solution is the technical term for the sterile liquid that carries the active ingredient, while Preservative keeps the bottle safe from contamination during repeated use. Understanding these basics helps you pick the right product and use it safely.
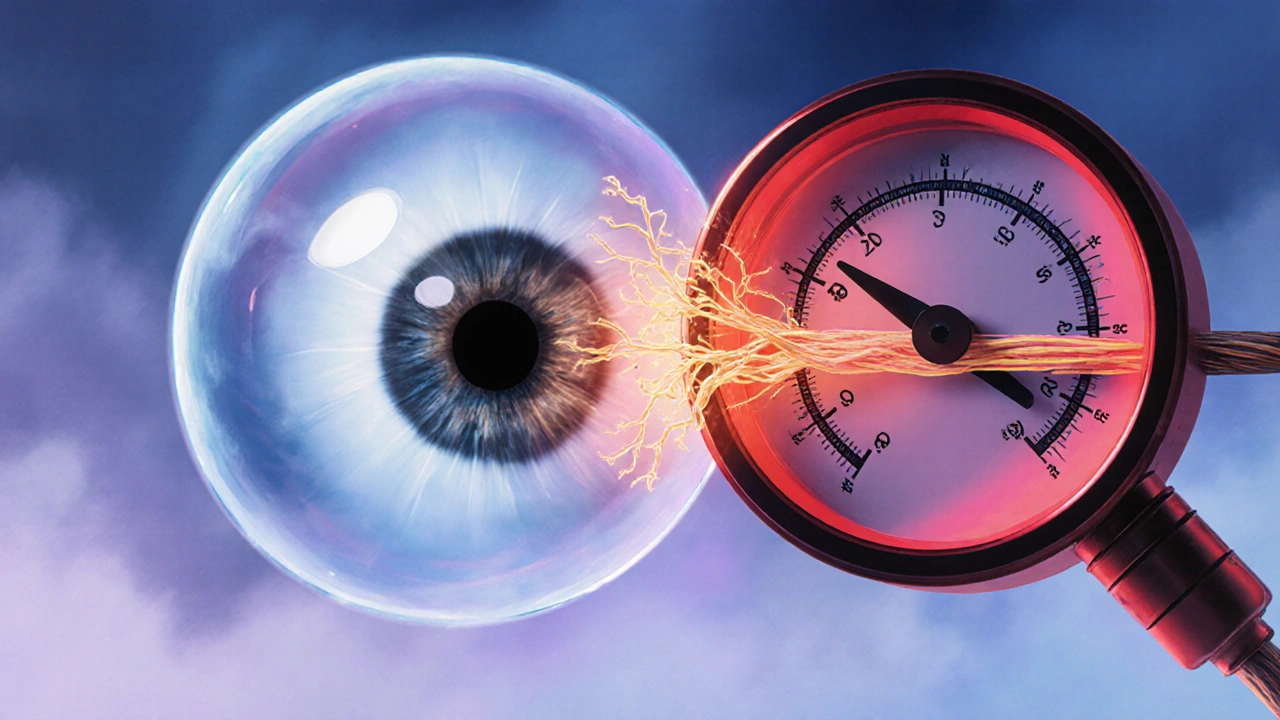
Eye drops aren’t a one‑size‑fits‑all product. The choice of eye drops depends on the condition you’re treating. For instance, Glaucoma demands pressure‑lowering drops such as prostaglandin analogs, while Dry eye benefits from lubricating formulas that mimic natural tears. Each formulation balances efficacy with comfort, and the preservative profile can affect tolerability—some people react to benzalkonium chloride, prompting a move toward preservative‑free options.
How Eye Drops Work and What to Expect
Eye drops work by placing medication right on the cornea and conjunctiva, where it can be absorbed quickly. This direct route bypasses the digestive system, so you often see faster relief compared with oral pills. However, the eye’s protective barriers mean the drug must be in the right concentration and pH to stay effective. That’s why manufacturers fine‑tune the Ophthalmic solution for each active ingredient, whether it’s an antibiotic, anti‑inflammatory, or steroid.
When you open a bottle, you’ll notice a dropper that delivers a measured volume—usually 0.05 ml per drop. The size matters because it determines the dose you receive. Too many drops can overflow, leading to waste and possible systemic absorption, especially with beta‑blocker drops for glaucoma. Follow the label’s instructions, wait a minute between different eye drop types, and gently close your eyes afterward to let the medication spread evenly.
Preservatives play a crucial role in multi‑dose bottles. They prevent bacterial growth after the seal is broken. Yet, they can cause irritation for people with sensitive eyes or chronic dry‑eye syndrome. That’s why preservative‑free single‑use vials are popular for long‑term dry‑eye therapy. Knowing the trade‑off helps you decide whether a preservative‑free product is worth the extra cost.
Beyond glaucoma and dry eye, eye drops treat infections, inflammation, allergies, and post‑surgical care. Antibiotic drops like ciprofloxacin target bacterial conjunctivitis, while anti‑histamine drops ease allergic itching. Steroid drops reduce swelling after eye surgery, but they require close monitoring because long‑term use can raise intra‑ocular pressure—a concern for glaucoma patients.
The article collection below includes deep dives into many of these drug classes. You’ll find comparison guides for antidepressants, nootropics, and even hair‑loss treatments—each of which can appear in an eye‑drop form for targeted ocular use. By linking the broader medication landscape to eye‑drop applications, the guides help you see how a single drug class can serve multiple therapeutic routes.
Now that you have a clear picture of what eye drops are, how they’re formulated, and why preservatives and specific conditions matter, you’re ready to explore the detailed articles that follow. Whether you’re curious about the safest options for dry‑eye relief or the best pressure‑lowering drops for glaucoma, the posts below will give you practical insights and side‑by‑side comparisons to make an informed choice.
Dorzolamide‑Timolol for Glaucoma: How It Works, Benefits & Use
Discover how Dorzolamide‑Timolol works, its benefits for glaucoma, dosing tips, side effects, and how it stacks up against other eye drops.